A Trial of a Novel modRNA Flu Shot: Not So Hot
We are pleased to publish this guest critical appraisal of a recent influenza vaccine RCT--from Johns Hopkins cardiologist, Dr Joseph Marine
Like many doctors, I am required by my health system to get an annual flu vaccine. It has never done me any harm, as far as I can tell. I will sometimes have some malaise and a sore upper arm for a day or two, sometimes nothing. Whether it has done me or anyone else any good is another question. Predicting the dominant flu strain in a given year is a guessing game, and the effectiveness of the vaccine has to be estimated from retrospective observational studies which are fraught with potential for bias and confounding.
In some years, the estimated efficacy is zero or less, as a Cleveland Clinic study found for the 2024-25 season. A 2018 Cochrane review found a modest benefit in reduction of influenza with vaccination of healthy adults, but there was little evidence of difference in other endpoints.
Importantly, in the matter of mandated vaccine for healthcare workers, another 2025 Cochrane review found “little to no effect” in nosocomial transmission in long-term care institutions when healthcare workers were vaccinated. Other studies have shown mixed results.
So I read with interest a recent study of a new modified RNA (modRNA) influenza vaccine published recently in The New England Journal of Medicine.
This study compared a novel modRNA influenza vaccine against a standard inactivated comparator vaccine in a randomized controlled trial of 18,476 subjects at 248 sites (mainly US) during the 2022-23 season.
The conclusion:
“The modRNA vaccine had statistically superior efficacy over the control vaccine, with greater immune responses to A/H3N2 and A/H1N1 strains but was associated with more reactogenicity events.”
Sounds like progress, but digging deeper into the study raised more questions:
1 Wrong Population and Potential Publication Bias
The study population was 18–64-year-old adults. But where were the 65-year-old and up group? The people who are most likely to get sick, get hospitalized, and die from influenza?
Turns out there was a 27,000-subject study in this age group with negative results that were not published, according to a report by Maryanne Demasi based on an interview with ACIP member Retsef Levi. This raises serious questions of publication bias and medical journalistic ethics. Cherry-picking “positive” results like this should be unacceptable. If the novel vaccine is not better in the group most in need of vaccination, what good is it?
2 Deceptive Endpoint and Data Depiction
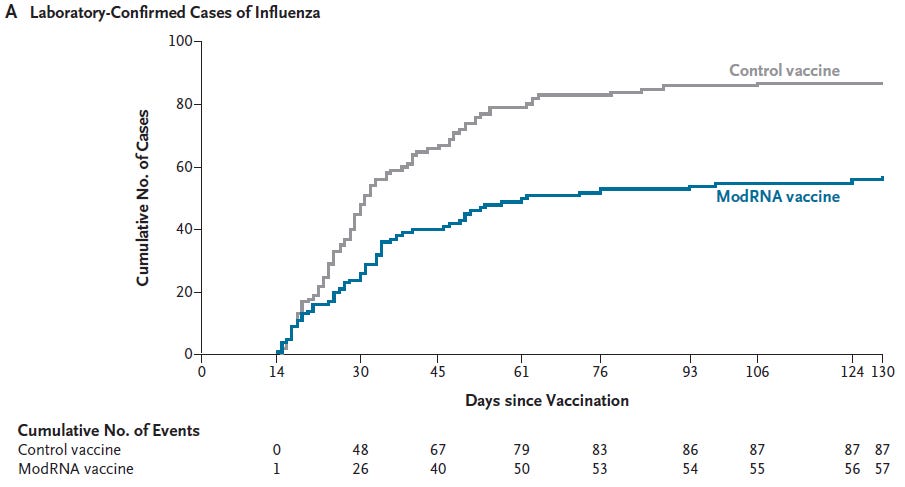
The primary endpoint was “laboratory-confirmed influenza associated with influenza-like illness (ILI).” This occurred in 57 subjects in the modRNA group and 87 control subjects. This was reported as a 34.5% relative efficacy for the modRNA product. The graph looks very impressive:
However, 57/9225 modRNA subjects = 0.62% and 87/9251 control subjects = 0.94% - so a 34.5% relative efficacy translates to only 0.32% absolute risk reduction (ARR) and a number needed to vaccinate (NNV) of 312.
Seen another way, both groups had a greater than 99% chance of getting through the winter without a case of laboratory confirmed influenza. Is this better than no vaccine? We don’t know, because there was no placebo control.
3 Adverse Events More Prevalent than Primary Endpoint
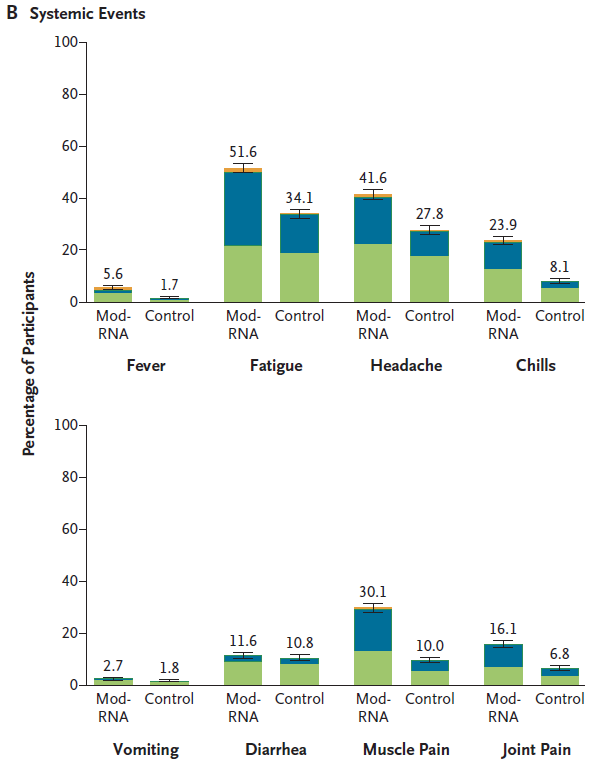
The report states that “adverse event profiles were similar in the two groups.” However, a closer look suggests that this is not the case:
You have to look at the y-axis carefully to see that it no longer represents individual subjects, but rather percentage of a much larger number of subjects: 5.9% of 9225 modRNA recipients had fever, representing an absolute number of 387 subjects more than controls.
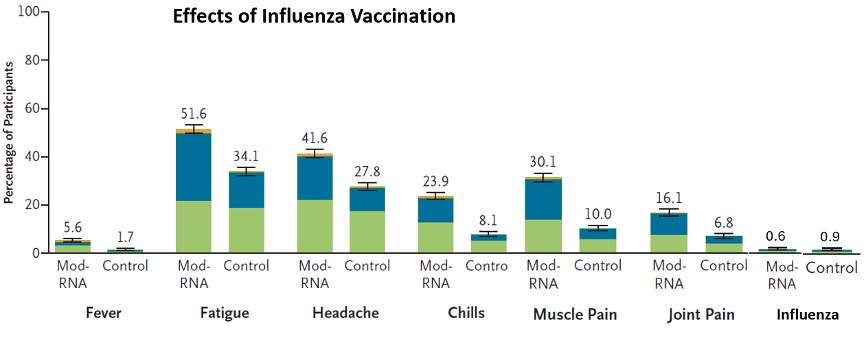
One can easily see that many more modRNA subjects had fatigue, headache, chills, muscle pain, and myalgias. If those symptoms sound familiar, it is because they are the symptoms of an influenza-like illness. The modRNA vaccine (known to be highly reactogenic) actually causes an ILI in apparently far higher number than there were actual cases of influenza. What good is a vaccine that causes the the same symptoms that one is trying to prevent?
To illustrate the deception of using different y-axes, I have added roughly approximate bar graphs for influenza rates to the systemic effects figure (see far right-sided panel):
4 Clinically Meaningful Endpoints Omitted
Flu vaccine recipients like me want to know if the vaccine will prevent them from getting sick (ie, reduce total influenza-like illness episodes), keep them out of the hospital, reduce days lost from work, reduce risk of death, and reduce the risk of spreading illness to others. None of these endpoints were analyzed.
5 Conflict of Interest
An added concern is that almost all authors were employees of the sponsor and as stated in the manuscript:
“The trial was designed and conducted by the sponsor . . . Representatives of the sponsor performed the collection, analysis, and interpretation of the data.”
There was no independent data monitoring board and there was complete industry control over assessment of all endpoints.
So we are left with a report of a novel vaccine technology that causes influenza-like illness in a high percentage of recipients and reduces actual cases of influenza only 0.3% with unknown effects on any other clinically meaningful endpoints – in a selected patient population of younger, healthier people at little risk of major adverse events from influenza.
Good for the FDA for rejecting this vaccine. These results also support RFK Jr’s decision to suspend more corporate welfare for modRNA vax development.
The public health establishment decried this decision, but this study shows that our $4 trillion pharmaceutical industry is capable of developing and testing novel modRNA products that they feel are commercially viable without more corporate welfare. It also shows that not every modRNA product is going to be a “miracle drug” and we should temper our future expectations.
FDA CBER Director (and Sensible Medicine co-founder) Dr. Vinay Prasad, in a recent internal FDA memo, has proposed bringing back randomized trials of annual flu shots. He has written about this idea previously. I hope he will succeed in doing so.
I would look forward to robust RCTs of future influenza vaccines with placebo controls and broad, meaningful clinical endpoints. I will be happy to volunteer for these future trials and I am sure many of my fellow health care professionals would as well.



Thank you. I believe that most people involved in healthcare and medical research are trying to do the right thing everyday. Sometimes our biases get in the way. We need a healthy and profitable pharma industry, but the mission of healthcare must always come first.
Excellent summary, thank you. As I recently noted (https://researchtranslation.substack.com/p/lessons-from-the-new-flu-vaccine) hiding negative studies while spinning others is straight out of the Pharma playbook. It worked well with Paxlovid, a still-profitable drug that failed every test. Best to think of a single, spun study like this as proof of failure, and unpublished studies as smoking guns. Well done, Dr. Marine.