"Before he gets chemo, he should go to the fertility preservation clinic". Docs say this, but is it true?
New research from my lab shows there is no evidence that this results in more kids
A few years ago, I was on service and about to start ABVD in a 20 year old man with rip roaring Hodgkin’s lymphoma. He had B symptoms, was hospitalized and deteriorating by the day. A colleague stopped me.
“Before you start chemotherapy, make sure he gets a referral to fertility clinic.”
“Why?” I asked.
“So he can bank sperm, if he wants. Either way, they must counsel him.”
“That will delay curative chemotherapy, and ABVD is less likely to result in infertility than people think.” I replied, “I have already discussed this risk with him, as part of informed consent, and he thinks proceeding now is prudent.”
“You have to refer all patients of childbearing age to fertility preservation.”
….
This happened to me, and is a common scenario in medicine. Doctors are increasingly pressured to refer to fertility clinic prior to chemotherapy. Words like “all patients of childbearing age” and “you must” are used. Obviously, since I am a scientist and physician, I had 7 questions that I wanted answered. So I asked Chris Eden and Alyson Haslam from my laboratory to answer them, systematically.
Just out in the journal of oncology practice, we have the answer.
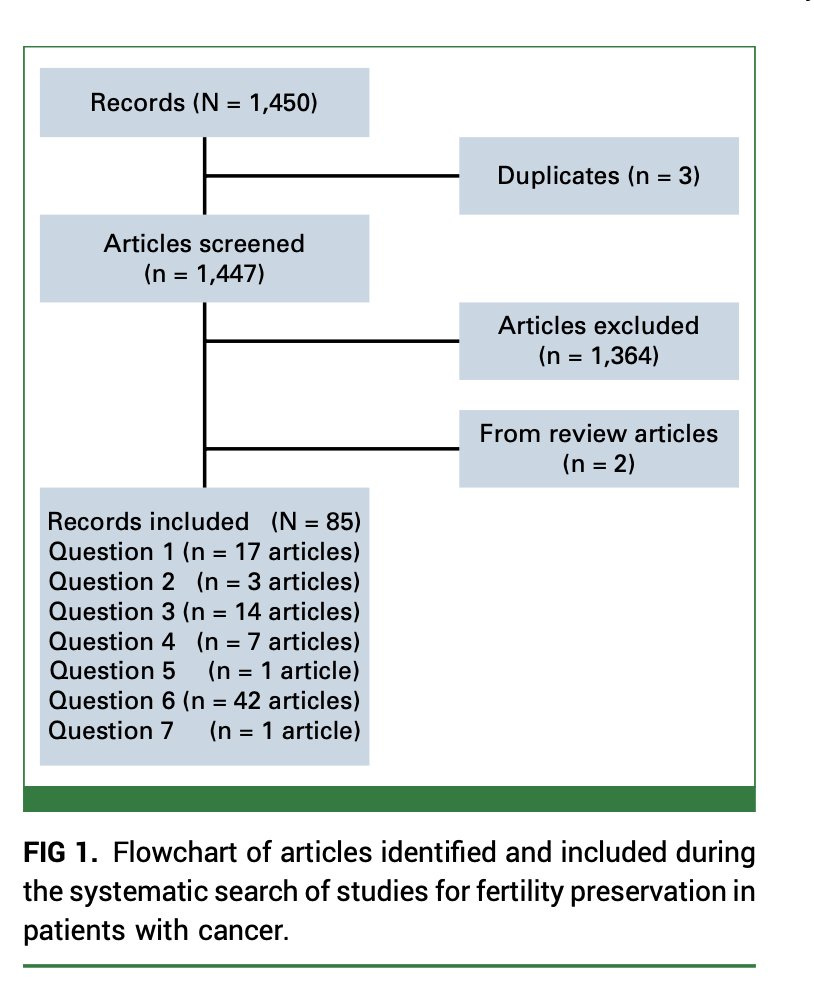
We searched the entire field and examined nearly 1,500 articles to find that 85 pertained to one of our 7 questions.
Just think about that. 1500 papers on this topic and only 85 try to answer 7 basic questions.
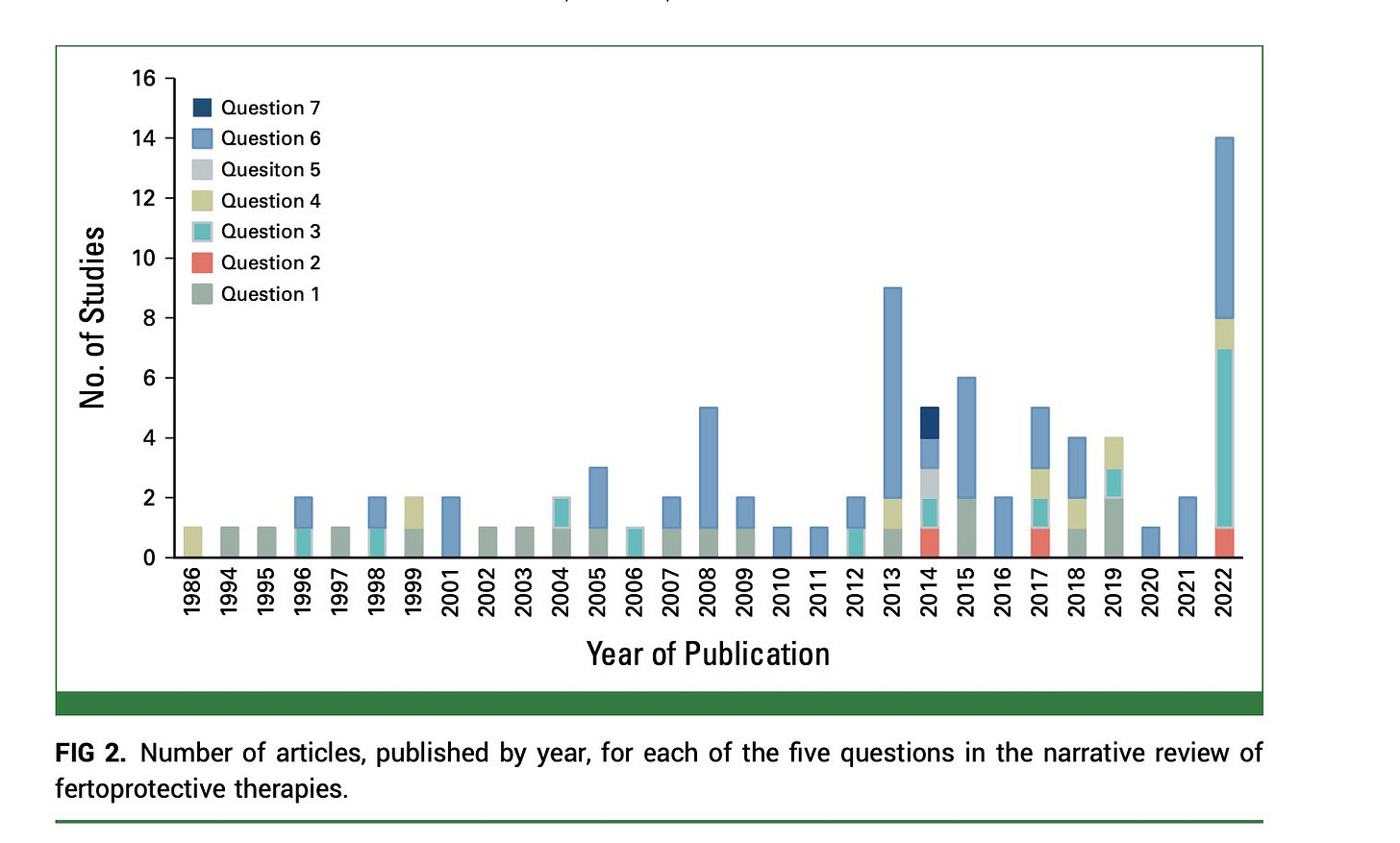
Here was the distribution over time.
Now for the questions. For the answer to all the questions, here is the full paper. Also attached at the end for subscribers.
I want to highlight the main finding.
These people. SMH. There are so many doctors who want to tell you how to practice medicine. They use moralizing language and are intrusive, but don’t seem to understand that you need to have data if you want to make universal recommendations. The idea that all doctors need to always refer all patients to oncofertility is unsupported.
There is no good evidence that this costly process results in more babies. Worse, it delays chemotherapy. The proponents are not even trying to assess if their recommendation makes people happier, or results in more babies. The evidence base is weak, and I searched clintrials.gov to find 0 useful ongoing studies.
This is 2024 medicine. A junior faculty member grows up in the school of activism. They are poor at critical thinking. They are happy to come and tell you that you need to wear a mask in the winter with your patients, refer for the annual covid vaccination, send patients of childbearing age to oncofertility, and perform breast MRIs if a woman has dense breasts.
What they are not interested in doing is generating any data that they are correct in any of these recommendations. They just want to make things up, and make everyone comply. Patients may or may not be better off, but they don’t care, they just want another issue to moralize about. Sadly, leadership and NIH fund them to pursue their unproven quality improvement.
Oncofertility has serious downsides. It scares patients into thinking treatment will make them infertile (not always the case). They end up banking sperm and eggs and delaying chemo. That might increase risk of death. They pay month over month a fee to keep those gametes refrigerated. And, at the end, we have no idea if they have more kids.
One person asked me, how do you account for the fact some patients may decide they don’t want kids? This is a power issue, but not a signal issue. You should still be able to see an effect. This is like intention to treat vs per protocol.
Another person said “fertility matters. people will pay 30k for a kid. Oncofertility is a deal.” Sure, fertility matters, but the question is whether we are selling snake oil. I could pay 30k to get a blood transfusion from a 20 year old to improve my vitality, but that is snake oil. Is oncofertility snake oil? Who knows. There are no data.
Oncofertility is feel good medicine. Masking 2 year olds in daycare with cloth masks made the American Academy of Pediatrics feel good. The key question in medicine isn’t: do you feel good? But rather: does this actually work?
For oncofertility the answer is: we don’t know. That just isn’t good enough. If I were a doctor telling other doctors what to do, I would either have good evidence, generate evidence or I would STFU. Too bad, that isn’t a universal ethic.