How to make a trial positive: Lessons from the PSMAfore Trial
We welcome Dr. Dries Develtere back today with another of our occasional letters to the editor. We publish theses since letters sent to the editors of journals have to pass through gatekeepers, take months to appear, are generally ignored, and do not lend themselves to discussion and debate. This letter addresses the PSMAfore trial originally published in The Lancet. I think it is an instructive piece of critical appraisal.
Adam Cifu
[177Lu]Lu-PSMA-617 (177Lu-PSMA-617) is a prostate-specific membrane antigen (PSMA)-targeted radioligand. It is presently used for patients who have PSMA-positive, metastatic castration-resistant prostate cancer who have already received an androgen receptor pathway inhibitor (ARPI) and taxane therapy. The purpose of the PSMAfore trial was to evaluate the effectiveness of this therapy in patients who had not yet received taxane therapy.
Trial Design and Methods
In this open-label phase 3 trial, taxane-naive patients with metastatic castration-resistant prostate cancer (mCRPC) who progressed on an androgen receptor pathway inhibitor (ARPI) were randomized 1:1 to receive either 177Lu-PSMA-617, the PSMA-targeted radioligand, or a different ARPI (abiraterone or enzalutamide). Crossover after progression on the second ARPI in the control arm to the PSMA-targeted radioligand was allowed. Accordingly, together with the final OS results based on the intention-to-treat (ITT) principle, crossover-adjusted OS analyses were presented.
Reported Outcomes
No difference in OS between groups was found in the ITT analysis. The crossover-adjusted analyses suggested that crossover confounded the OS results. When adjusted for crossover,results favored the group treated with the PSMA-targeted radioligand with hazard ratios ranging from 0.54 to 0.62. The favorable safety profile of the PSMA-targeted radioligand compared to another ARPI—with fewer high-grade adverse events, longer time to worsening in health-related quality of life (HRQoL), and longer time to symptomatic skeletal events—had already been published (here and here). The current final analyses confirmed the acceptable safety profile with no new signals.
Concerns Regarding the Control Arm
There is, however, significant concern regarding these conclusions given the choice of a suboptimal control arm. It is well established and acknowledged by the authors themselves in their introduction that ARPI switch in mCRPC is associated with cross-resistance and is consequently not the most effective treatment in this setting.
In practice, the next step in therapy would be to offer patients taxane-based chemotherapy. This, therefore, should have been the control.
Defending the Control Arm: Limitations of the Argument
To defend this choice of control, one must argue that some patients wish to defer or avoid chemotherapy. However, supplementary figure S4 contradicts this justification: no difference in time to chemotherapy was observed between both arms (ITT groups) with a hazard ratio of 1.07 (CI 0.86–1.35). Moreover, patients who crossed over from ARPI to 177Lu-PSMA-617 actually had a longer time to chemotherapy, further undermining the argument that chemotherapy deferral explains the design.
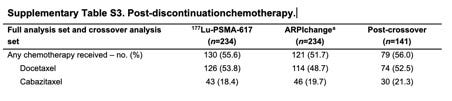
We can take it even further if we look at Supplementary Table 3 about post-protocol therapy: no significant difference between the groups. If we are being really strict, you can actually see that more patients in the PSMA-targeted radioligand group got chemotherapy compared to the control group.
Missing Representation of Frail Patients
Another justification provided was that some patients are ineligible for taxanes due to age or comorbidities. However, such patients were not represented in this trial, which included only patients with an ECOG score of 0–1 and adequate organ function. This represents a missed opportunity to investigate the tolerance of the PSMA-targeted radioligand in more fragile patients—the very population the authors themselves identified as most in need of an alternative to second ARPI.
Implications for Overall Survival and Standard of Care
It is widely accepted that a new drug should demonstrate OS and/or QoL benefit compared to the standard of care. In the PSMAfore trial, the PSMA-targeted radioligand failed to improve OS compared to a suboptimal control arm. No conclusions can be drawn about its effect on OS relative to standard or care chemotherapy. Although crossover may have confounded the ITT OS analysis, the absence of standard of care in the control arm means the trial only shows survival benefit versus second ARPI, not versus the standard of care.
Interpretation of Safety and QoL Outcomes
A favorable safety profile and longer time to worsening in HRQoL compared to a treatment with known cross-resistance to the drug that patients are progressing on is to be expected. If patients are experiencing symptoms in the first-line setting due to progression, and are receiving an ineffective drug in the second-line, those symptoms will not improve.
Conclusion
So, to conclude, what was the intention of the PSMAfore trial?
The trial wanted to investigate if the PSMA-targeted radioligand177Lu-PSMA-617 could offer
a rPFS and OS benefit compared to ARPI switch
in patients who wish to defer or avoid the toxicities of chemotherapy
or in patients who are ineligible for chemotherapy due to age or comorbidities
What did we actually learn from the PSMAfore trial?
There was an rPFS benefit but no OS benefit
In both groups, the number of patients receiving chemotherapy and the time to chemotherapy were the same
Patients ineligible for chemotherapy were not included in the trial
This means that the intervention arm did not demonstrate a clinically significant benefit compared to a suboptimal control arm.
The authors conclude that this trial supports 177Lu-PSMA-617 as an alternative treatment option to ARPI change for patients who are considered appropriate to delay taxane-based chemotherapy.
I conclude that ARPI change should almost never be an alternative treatment option and definitely not a control arm, and that chemotherapy was NOT delayed in these patients.
Knowing this, why is the tone of the manuscript this positive?
I think I know the answer:
Dries Develtere, MD, is a Urologist at the General Hospital of Ypres, Belgium. He specializes in robotic surgery, with a focus on prostate and bladder procedures, as well as urological oncology. He is the founder of Surgical Vision, a video platform that provides high-quality surgical training videos designed to advance surgical education.





Excellent appraisal by dr Develtere. Fully agree. Please also see:
https://www-nature-com.proxy-ub.rug.nl/articles/s44276-024-00065-7 and
https://www.drugdevletter.com/p/lu-psma-and-the-need-to-educate-medical
Maybe after reading titles of studies we should skip ahead to see who is funding the study and then go back and read the results. Kidding..not kidding.