I May Have Been Too Enthusiastic About the FRAIL AF Trial
Study of the Week: A new analysis of switching from warfarin to DOACs makes me question my initial enthusiasm for the small Dutch trial
Last week, a group of authors from Boston published a clever analysis of the DOAC vs warfarin trials in an effort to replicate the FRAIL AF study—which tested the question of whether older patients with frailty should be switched from vitamin K antagonist (VKA) to direct acting oral anticoagulants (DOAC). (Note: the most common VKA in the US is warfarin, but in Europe, a drug similar to warfarin called phenprocoumon is also used.)
FRAIL AF excited me because it was a great effort from curious investigators, and because it found that switching to DOAC led to a highly significant 69% increase in major bleeding. This was a surprise because a presumed advantage of DOACs over VKAs is safety.
Yet FRAIL AF studied patients who would not have been enrolled in the seminal trials. The findings further supported my view that evidence derived in patients healthy enough to be in a major trial should be translated to older patients with multiple conditions with great caution—if at all.
The new analysis makes me think I was too enthusiastic about FRAIL AF. I cover these two studies as lessons in evidence appraisal and humility.
The New Study
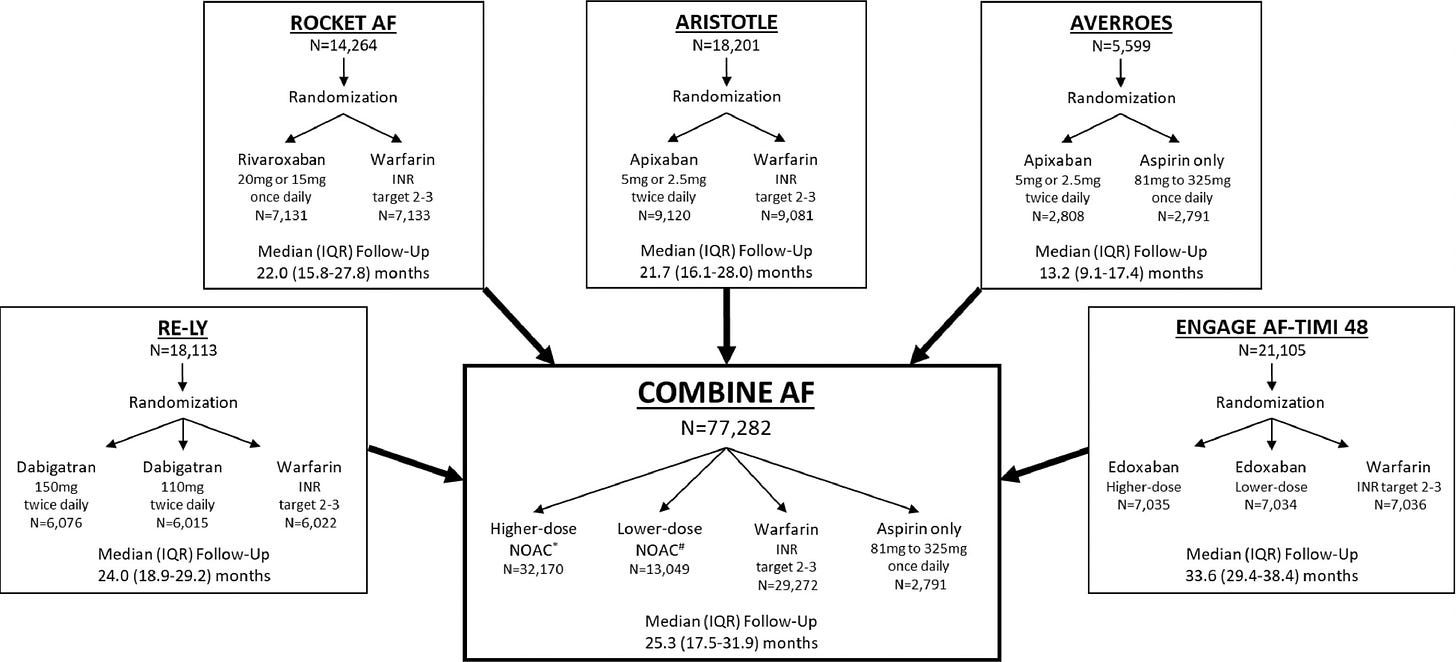
Authors from the big four DOAC vs warfarin trials have collaborated to share patient-level data. The COMBINE AF collaboration is a powerful dataset comprising nearly 77,000 patients in the RELY (dabigatran), ROCKET (rivaroxaban), ARISTOTLE (apixaban) and ENGAGE AF-TIMI (edoxaban) trials. You can do a lot with this sort of data:
For this clever substudy, the authors took patients who had three criteria:
Older than 75 years
Positive markers of frailty
Were on VKA at trial entry—the so-called VKA-experienced group
These nearly 6000 patients, the authors presumed, were FRAIL-AF like patients. Then they assessed outcomes depending on random group assignment. About 3000 were kept on VKA and the other 3000 were randomized to DOAC (switched group).
The authors also looked at patients without all three of these characteristics. There were nearly 52k of these patients.
Main findings:
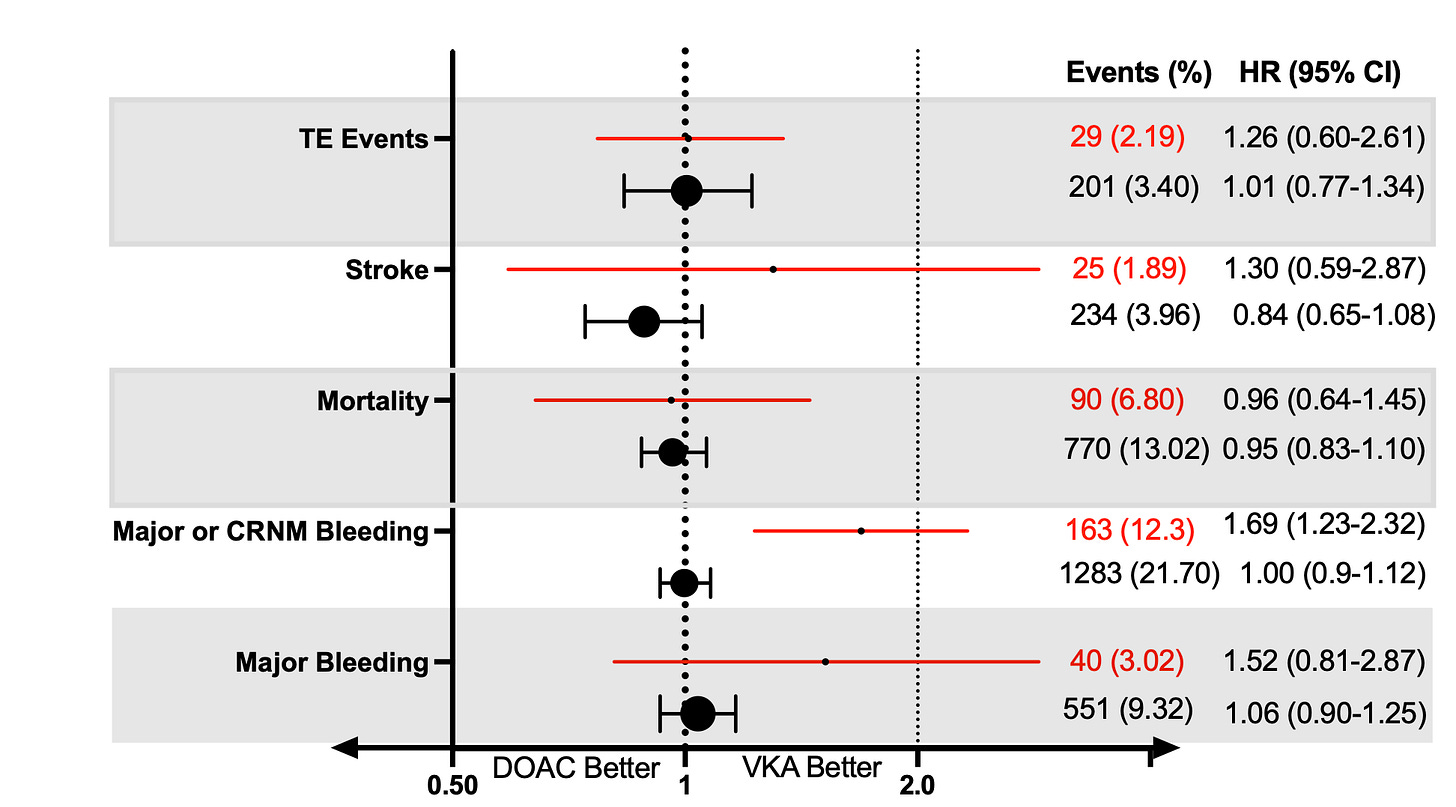
In the FRAIL AF-like patients, there was…
a 17% relative reduction in stroke and systemic embolism that did not reach statistical significance. [HR 0.83 (95% CI 0.65-1.07)]
no difference in all-cause death [HR 0.95 (0.83-1.10)]
no difference in major bleeding [HR 1.06 (0.90-1.25)]
no difference in net clinical outcome (combining efficacy and safety) [HR 1.01 (0.91-1.13)]
In the larger group of patients without the three FRAIL AF-like features, switching to DOAC led to statistically significantly lower rates of stroke, death bleeding and a net clinical benefit. This is what the DOAC vs warfarin meta-analyses have found.
The tension between the two studies
FRAIL AF was stopped early because of higher rates of bleeding in the switching arm. COMBINE AF found no signal of increased bleeding when VKA-experienced patients were randomized to DOAC.
I see three reasons why the study results may have varied.
First is that measures of frailty may have led to different patients being enrolled. The two studies used different frailty scales. COMBINE AF authors did not have some of the frailty measures available in the FRAIL AF trial. For instance, FRAIL AF had measures of social isolation, not available to the COMBINE AF group.
The second reason for the different findings may have been specific to the DOAC drugs. In FRAIL AF, the group that switched from VKA to DOAC mostly started rivaroxaban. The exact mix was rivaroxaban 54%, apixaban 19%, edoxaban 18%, or dabigatran 9%.
The COMBINE AF authors ran a simulation with this exact mix. Remember, they had patient-level data in 77k patients. With this simulation, they found a statistically significant 22% increase in major bleeding, and a 2.2x increase in GI bleeding. The COMBINE AF authors then did a second simulation with only apixaban and edoxaban and found a 17% reduction in major bleeding. While simulations are not definitive, there is, at least a suggestion, that specific drugs may have mattered.
The third reason is the most persuasive. It was power. In the FRAIL AF study there were only 40 major bleeding events vs 551 events in the COMBINE AF trials. Look at the error bars and confidence intervals below.
I realize that I sound like a broken record, but small numbers of events reduce confidence. Perhaps the trials were different (frailty scales and drug combinations), but I would put my money on numbers of events.
This does not diminish FRAIL AF. It’s still a remarkable effort. We need more FRAIL AF-like efforts in medicine.
But we also need to be careful with small numbers of events. Results need to be replicated, preferably in multiple trials.
The clinical translation of these two studies is easy:
For elderly frail patients on warfarin, I don’t think we are mandated to do one specific thing. FRAIL AF said don’t switch when doing well on warfarin. COMBINE says that if you switch, outcomes are similar. There is not a major advantage or disadvantage.
But if an elderly frail patient wanted to switch, say, to decrease the work of being a patient, COMBINE AF results would argue that outcomes would be similar.
Hence: switching should neither be proscribed nor recommended. It can be a shared decision with the patient and his or her family.
As of this morning, Sensible Medicine is a handful of subscribers short of 100,000. I would have never imagined this when we started this project. Thank you. JMM


I have a strong preference for apixiban (Eliquis) in the elderly. Apixiban was approved a year after rivaroxaban and became my preferred DOAC thereafter because of the more sensible dosing (2.5 mg if. 2 of following, >80 years, <60K, creatinine >1.5 mg). In addition, apixiban was superior to warfarin in lowering ischemic stroke with less bleeding risk, whereas rivaroxaban wasn't in the major RCTS (ARISTOTLE and ROCKETAF) establishing their efficacy. Clinicallly, I've seen much more GI bleeding on rivaroxaban (generally not prescribed by me) than apixiban.
Warfarin management is the key to safety with VKA in the frail elderly. I ran a warfarin clinic for a decade and our time in therapeuti crange was much higher than that in the major AFIB trials with a correspondingly lower rate of major bleeding. Conversely, I've seen quite a bit of bad management of warfarin when managed by individual docs based on blood draws.
I've also had patients who obsessively manage their warfarin dosing with at home PT tests who do wonderfully for decades.
Every patient is different and discerning docs take into account how well the warfarin management is for the individual and if not ideal, switching to the best and safest DOAC
We need more clinicians across the board who can critically re-examine their opinions and change them. No applogy, just diving in with an open mind and correcting the assumptions. Thank you for the reminder, Dr. Mandrola.