Is there a such thing as 'too little benefit' in oncology?
And is there a price we can't afford?
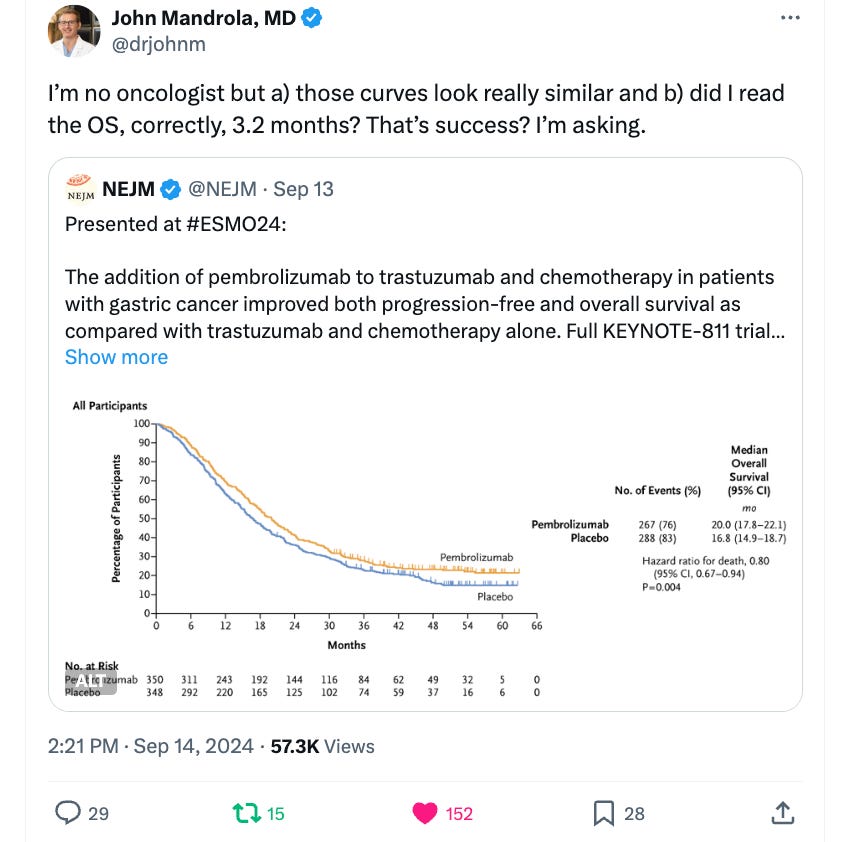
Recently John Mandrola, once again, stepped out of his lane. About a recent, cancer trial, which was celebrated by oncologists, he said this:
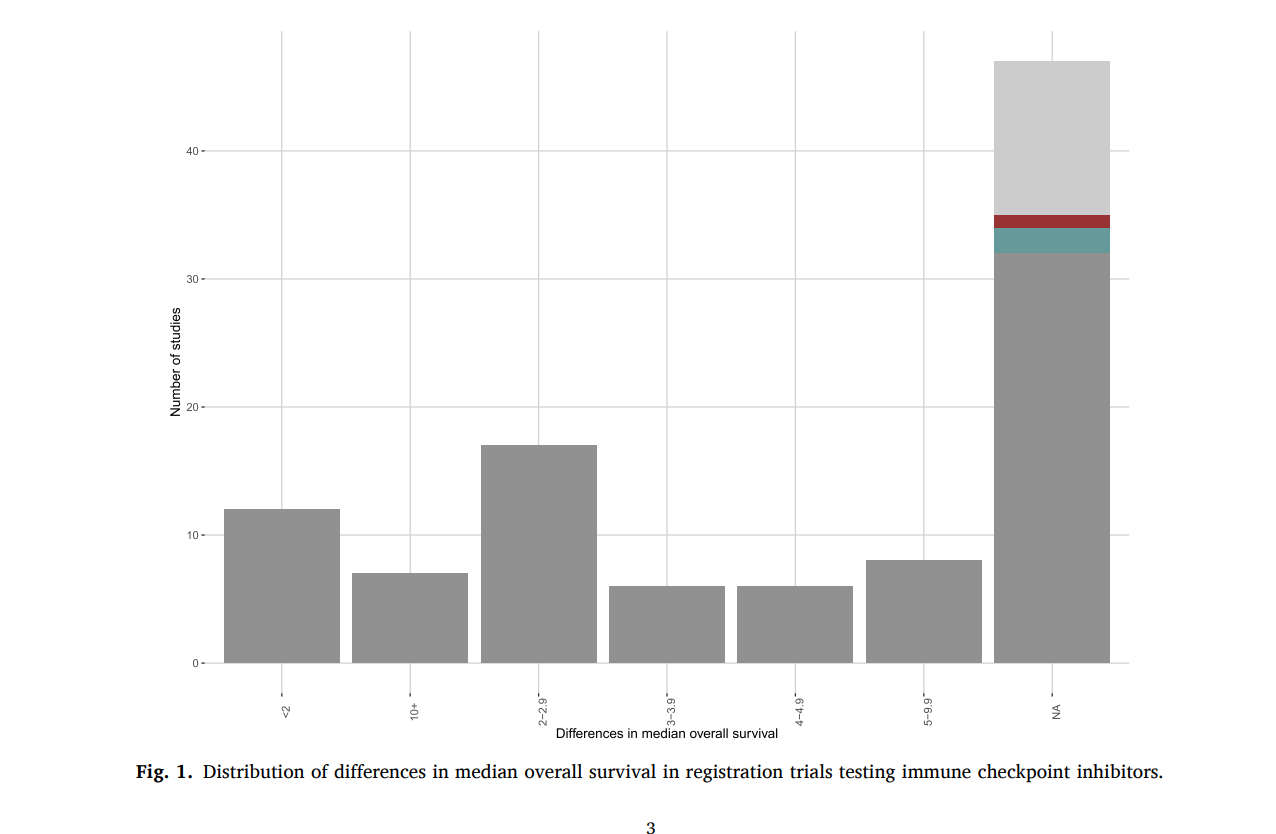
In fact, John’s observation is broadly true for this revolutionary class of medications. Although these drugs— checkpoint inhibitors— are great for melanoma and cutaneous squamous cell cancer, they aren’t wonder drugs and many uses are marginal. Here we quantified the benefit across all drug approvals.
Look at all the trials with <2. The reason there are so many N/A is because the company did not run randomized trials.
And, let me add one more detail. These drugs often cost 200,000 per year of treatment.
John is absolutely correct to ask whether, as a society, we should be spending so much money for so little, especially when cancer patients deserve better. But his finger isn’t exactly on the pulse of oncology. Most oncologists are happy to see ANY survival benefit. The results above will be incorporated into every US practice. That isn’t the edge of the debate.
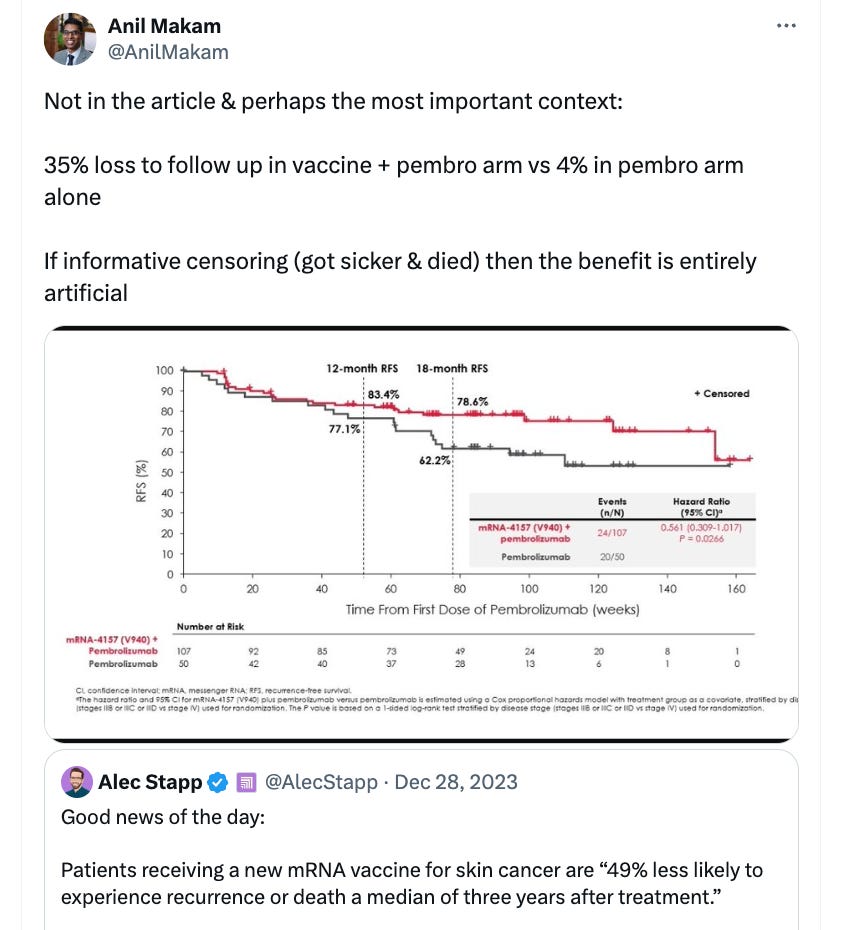
Instead, the edge is must further. Doctors are debating— as we speak at the European Society of Medical Oncology— whether to offer drugs that don’t improve survival.
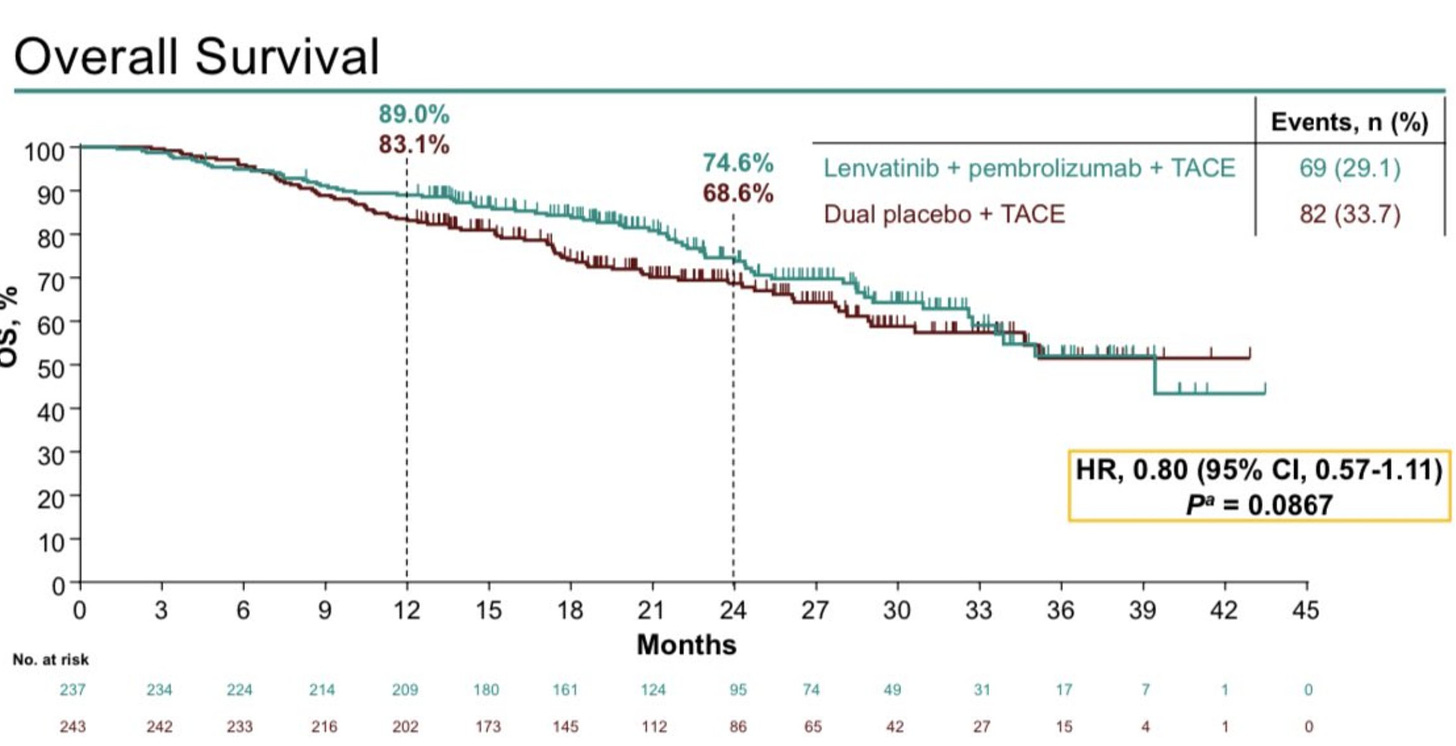
Take a look at this:
This trial is negative, but many oncologists on social media praised these results. The discussant called it a new standard.
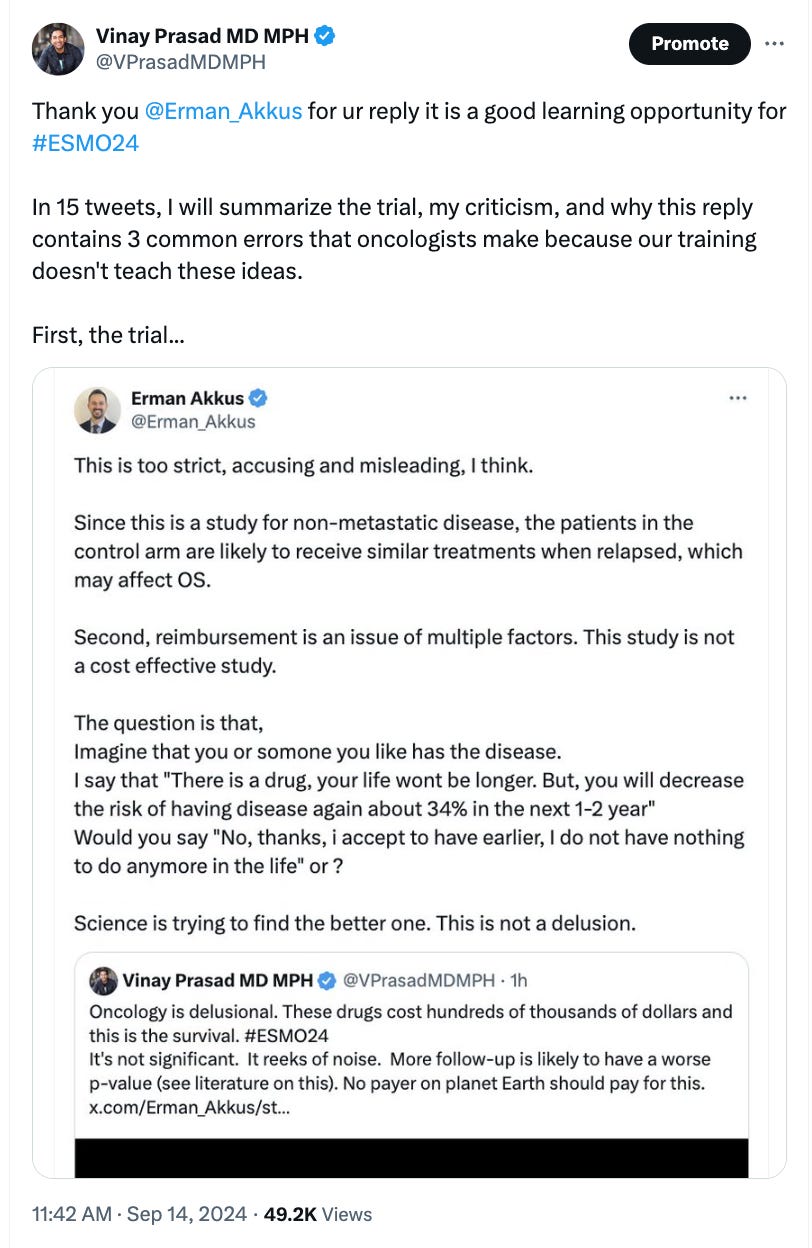
I had a spirited back and forth with one proponent, where I explained why the results were incorrect. It’s worth your time; click the link.
At one point, my interlocutor even argued….
I don’t think that is true. Most of us would rather leave a billion dollars to our children, and worse: I don’t think that this can be true when we ask others— Medicare and insurance companies— to foot the bill. No society can pay billions for one person, one drug.
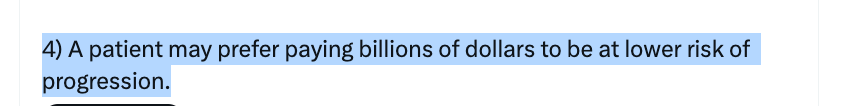
Here is Dr. Javid, an ID doctor.
Sometimes oncologists need a reality check from non-oncology physicians.
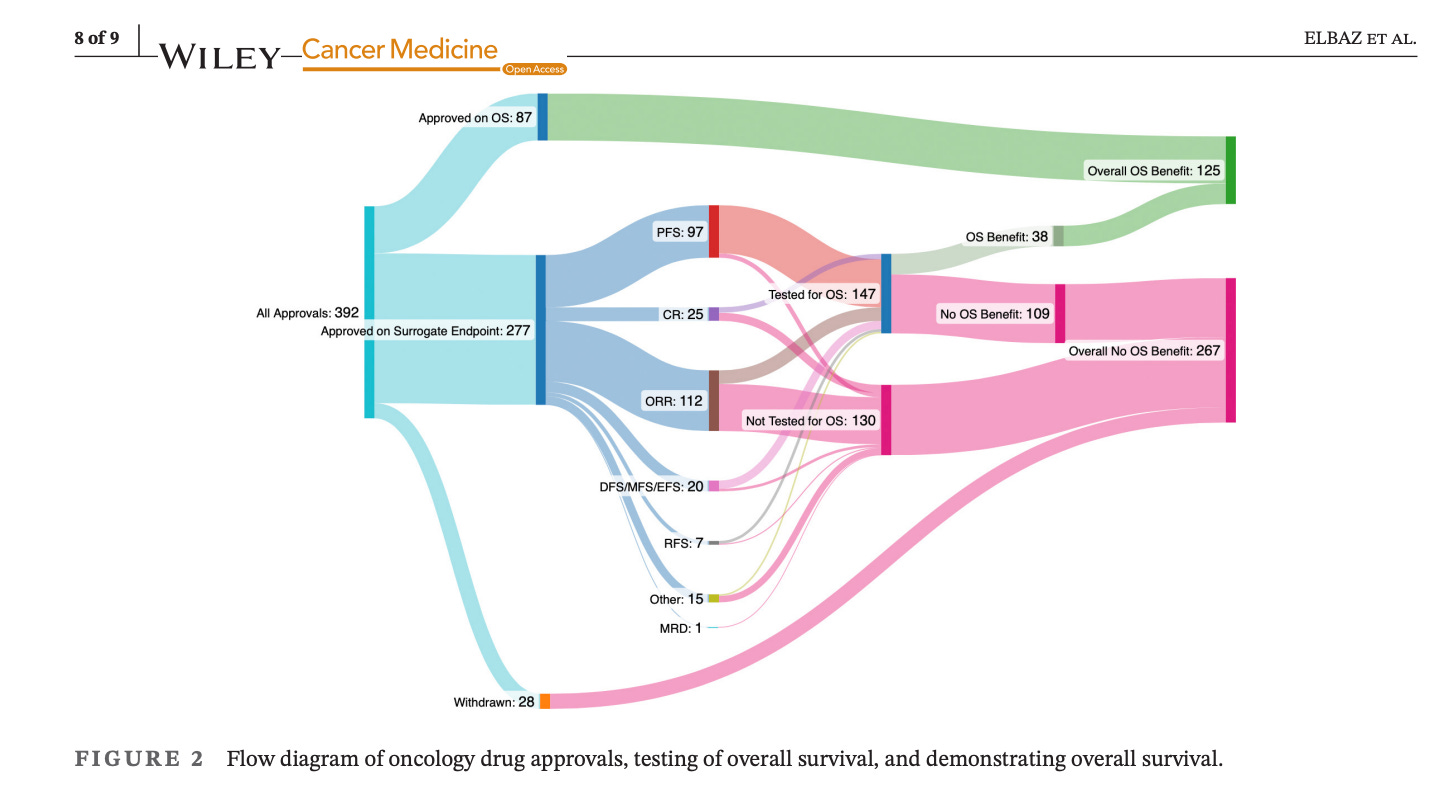
In another analysis, run by my lab. We analyzed the fate of 392 drugs approved by the FDA in oncology.
Just 125 drugs improve survival! 267 have never shown this, and 109 are known not to!
Oncologists need to see a psychiatrist.
Why does this happen? Why are oncologists adamant that 3 months survival benefit at a price of 200,000 is worth it, and even pushing to pay 200,000 for 0 days survival benefit, as long as CT scan are mildly better? I believe it is 5 factors
Financial capture. Oncologists (in the US) make more money, the more drugs they give. 4.5-6% of the drug cost goes to the center that infuses outpatient therapies, and these monies flow back to doctors— even in bigger hospitals and universities. Moreover, many expert doctors take payments from pharma. Although they don’t think these payments influence them, they do. Financial conflict is a form of corruption, in my opinion.
Poor critical thinking skills. Oncology training programs spend ~0 time teaching oncologists how to critically read the literature. That’s partly why I wrote the book Malignant. Oncologists are extremely vulnerable to propaganda and can fall victim to incorrect ideas when they are not equipped with strong critical thinking skills.
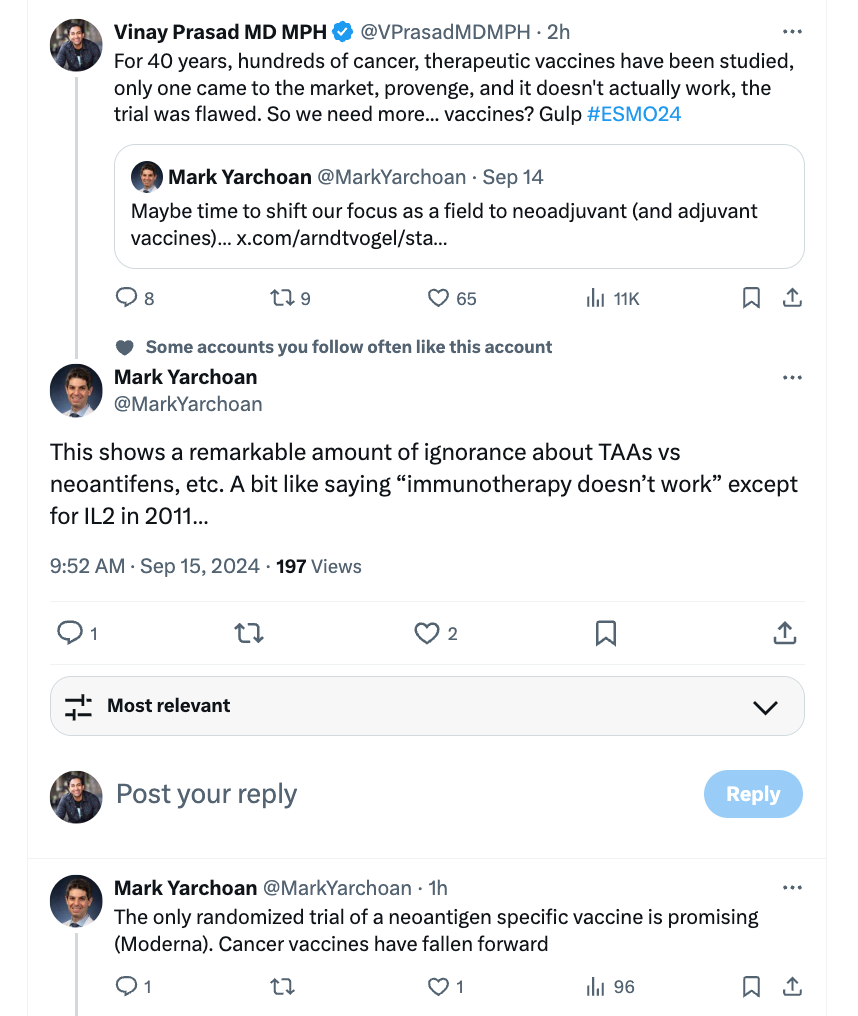
We want to believe. Treating people dying with cancer can be difficult, and we want to believe we are living in an age of remarkable progress. Recently another oncologist said I was remarkably ignorant about the promise of cancer therapeutic vaccines. He cited a new one by Moderna.
But that trial he discussed had huge problems. Anil Makam, a non-oncologist, saw them.
We believe in mechanistic science. During the pandemic, many people kept taking about some dummy— I mean mannequin, this is not ad hominem— which sprayed fewer particles with a cloth mask on than no mask. But whether or not mask mandates work is a bit more complicated than a dummy spraying particles. The same is true for cancer biology. Whole meetings are devoted to mice and cell lines and these have nothing to do with people. All drugs have a pre-clinical story that is promising, most fail.
Groupthink— the oncologists who fall victim to the above pitfalls want to live in groupthink. They aren’t willing to debate, or invite serious criticism at their conferences. I think this trend is continuing in society— where no one wants a good verbal joust. As such, many oncologists only hear the same propaganda.
Ultimately, I am grateful when oncology outsiders like Dr. John Mandrola point out that the emperor has no clothes. We need to hear it in oncology. Sadly, I think the ultimate solution will not come from internal self-regulation. Congress or the executive branch is needed to put the sense back into oncology; just as sensible medicine is needed to put the sense back into medicine.
Subscribe to support our mission



So my best friend became horribly depressed a few months ago. We had just come back from watching Michigan win the championship and staying at the team hotel with my nine-year-old grandson. We met the entire team. he never mentioned the headaches.
He went to his pcp and was given meds . I asked for a CT (doc refused) . A week later he "forgot how to walk" . His wife took him to our heart hospital and 30 min later he had the dx of GBM. My neighbor is oncologist and saw him and said leave Austin. Go to Chicago where they are aggressive doing surgeries while awake to maximize resection and minimize disability. The care locally was basically the same medicine they used since 2005, CT scans in a few months and then hospice. This was sort of this summation of my oncology colleague . It's out of my wheelhouse obviously.
He's now had three surgeries and two cyber knives since diagnosis. His complex imaging shows no active tumor for now.
On the way to Chicago we saw another 44-year-old bald man with multiple scars. He lives just a few miles from my house and we met him. He has five children and now is status post three surgeries and is cancer free. He is two years post diagnosis.
So we're living in real time with this. I am a cardiologist retired and I flew to Chicago with his wife to meet the team. My best friend had taken no medicines at age 72 prior to this diagnosis .
I wanted to be sure he wasn't going to get on the train to nowhere filled with chemo that we used to call "rocket fuel" in residency. I am 67 and I know advances are amazing in all aspects of medicine even in my lifetime, but reading this article reminds me of "rocket fuel" of the past.
Rather than hospice, they always came up with something which had horrible side effects and led to the same outcome.
I could not become an oncologist and God forbid a pediatric oncologist.
I was incredibly impressed with the Chicago team. It was medicine the way it should be. They review all the images done on Monday radiologist, oncologist, and surgeon.
On Tuesday, you sit in room with those three physicians high-tech screens both to look at images and to draw pictures as well as social workers and the nurse practitioners who are your case managers.
They spent over an hour with us reviewing the ideology of Glioblastoma, which, interestingly, they believe has a relation to pollution and nasal inhalation. It appears the one good part about growing up with bad allergies and constant runny nose is it reduces your risk they believe of this horrible disease.
They believe the disease sort of takes a life on its own. It fights back and they use a combination of advanced genetic analysis, frequent imaging and surgery done under local anesthesia. That's correct local anesthesia to remove the tumor.
The program is funded, obviously giving them the time to truly have a team to sit in the same room and discuss and manage patients. It's a far cry from my neighbor seeing 40 patients a day.
So where does randomized large control trials come in ?
Ideally, as often as one can but at the same time if we're going to be aggressive with these devastating diseases, I would think we should spend funds to create the centers of excellence and pay for the travel.
I think the biggest problem is that people do want to believe that they can stop death and they do not realize the cost. The pricing system is so screwed up because in order to get $50 doctors must charge Medicare $100. When people see the bill for $200,000 but Medicare only pays $30,000 they have no idea the true cost. I do not believe it is the financial wants of the oncologist. Because oncologists had to join in groups just to afford to buy the drugs, they no longer know the financial incentive. They are now employees. The Affordable Care Act had so many adverse effects on the healthcare system.