A new English study by Nafilyan et al published in Nature Communications has revived a heated debate about what we do and don’t know about cardiac adverse events following mRNA vaccination -- specifically about how often they are fatal. With some countries, such as the US, continuing to recommend mRNA vaccine boosters for very low risk populations, this remains a highly relevant topic and will likely continue to be for years as people look back on what we knew when about the safety of COVID-19 vaccines.
Autopsies and case reports can only provide their best judgement about whether a death is vaccine-related. Population-level data is also challenging to use to show with certainty there is a signal indicative of vaccine-related deaths when the magnitude of the increased deaths from the expected baseline death rate is relatively small.
Myocarditis was a much easier vaccination safety signal to detect, particularly in young males after dose 2, for example, where the observed vs expected rates of myocarditis post vaccine were already early on, even using numbers reported by the FDA, around 100 fold greater, if not more, than expected in the immediate post-vaccination timeframe.
Demonstrating much smaller observed-to-expected ratios requires diligent work. Believing you are seeing more reports of sudden cardiac deaths in the news recently, for example, just won’t cut it (are you paying more attention? Are they being reported more frequently? Are athletes at higher risk for other reasons? Is it really higher and if so, how do you know?... many people, thankfully, understand all of this intuitively).
The new Nafilyan et al paper is a very careful and impressive analysis of population-level data from English 12–29-year-olds. It uses the self-controlled case series design, which I have discussed before. But briefly, in this type of study, all patients experience the event (death) and have the exposure (vaccination), so the question is how does the risk change post-exposure. And, in this way, patients act as their own controls.
For this post, I interviewed the senior author of this study, James Doidge, specifically about their findings of cardiac death risk post mRNA vaccines in young males. He is a senior statistician and an honorary associate professor at the London School of Hygiene and Tropical Medicine. But before I get to that and the new study’s findings, I want to review what we already know about the cardiac risks of mRNA vaccines because I think it gives some important context.
Background
It is now widely accepted that the COVID-19 mRNA vaccines cause myocarditis. This is around 8-10x more common in males than females and is about 2-7x more likely after dose 2 than dose 1. It occurs at an estimated rate of 1/2700 post dose 2 Pfizer vaccine in 12–17-year-old males according to prospective data from Hong Kong (where all were hospitalized) and up to 1/1300 after Pfizer-Moderna combination for dose 1 and dose 2 according to data in JAMA Network Open from Canada in 18-24 year old males. It also occurs after the Pfizer booster at a rate around 1/6800 in 18–39-year-old males according to a very carefully-done study from Kaiser Permanente.
There are a limited number of people who continue to insist post-vaccination myocarditis is “mild”. I do think we have some evidence from the Nordic countries that post vaccination myocarditis may on average be milder than classic myocarditis (though important questions about the study are yet to be answered), but that does not mean it is always mild, nor does it mean you want your own child to get it. According to CDC data in Lancet Child & Adolescent Health, among 12-29 year olds with post-vaccination myocarditis, one had received intensive care requiring ECMO, but on average, at 90 days post diagnosis over 25% were still taking medications for the myocarditis diagnosis, over 30% were still on activity restrictions and 54% still had at least one abnormality noted on follow up cardiac MRI. And most of these young people had no underlying health conditions and thus faced exceptionally low risks from COVID-19 to begin with.
Reasons for these 3-6 month activity restrictions include the potential to prolong recovery and increase risk of sudden cardiac death acutely. But even after the first 6 months, there is felt to be a longer-term risk of sudden death from myocarditis due to arrhythmias, likely from scar formation. The presence of abnormalities on cardiac imaging (specifically late gadolinium enhancement [LGE] on cardiac MRI) has been strongly associated with worse prognosis in classic myocarditis. Concerningly, this LGE was identified in around 70% of post mRNA vaccination myocarditis after 3-6 months (according to one study of 12-17 year olds). There was a recent published case of an mRNA vaccine associated myocarditis in a 46 year old male who 7 months after initial diagnosis went on to develop ventricular tachycardia and an implantable defibrillator was placed; the true rate of long-term complications from mRNA vaccine-associated myo/pericarditis is yet to be determined.
Post-vaccination myocarditis occurs with a range of severity and symptomatology:
Subclinical myocarditis (with no or symptoms too mild to seek care) has been estimated to occur in about 2.8% of Swiss healthcare workers and 3.5% of 13–18-year-old males post Pfizer dose 2 the implications of which are unknown. Pfizer has yet to provide the FDA with requested data on subclinical myocarditis post vaccination.
Suspected/”probable”/”likely” fatal cases have been reported for example from Israel in NEJM, from the US in NEJM and peer reviewed reports from South Korea, after a booster dose in a 14 year old girl from Japan and in adults 46-75 years old from Germany). The last of these: autopsy reports from Germany were interesting because:
The autopsies found a unique pattern of myocarditis with the same sort of T cell dominant lymphocytic infiltrate and
Those autopsied had not sought medical care and would not have been counted as myocarditis cases in national databases or studies had they not had autopsies performed.
To summarize, we know classic myocarditis can be fatal (short and long-term) and post-vaccination myocarditis exists on a spectrum of severity; some cases require ICU care including requiring ECMO and there have been numerous deaths from myocarditis which were felt to be “likely” or “probably” attributable to the vaccine, even among some who did not seek medical care.
New English Study
Enter the SCCS study from England, which tries to answer the question: are young people dying in a way that is temporally related to their vaccination, how often, which vaccines, which doses and is it specifically from cardiac death.
They look at 12–29-year-olds in England – a pool of around 1.5 million young people and specifically analyze 1956 deaths linked to vaccination records from 12/8/2020 to 3/31/2022 and then separately look at 3219 registered deaths linked to a SARS-CoV-2+ test from 12/8/2020 to 12/31/2021. They use a self-controlled case series (SCCS) method to explore the risk of death following vaccination or SARS-CoV-2 test in the subsequent 12 weeks and compare that with a “baseline” period which they chose to be any time after 12 weeks. This study looks at shorter-term risks (over the course of 12 weeks) and compares those to a period of more long-term risks (which can go up to as high as 70 weeks depending on when a person’s first dose was).
As stated above, this type of study design is well-suited for investigation of vaccine safety signals because you select only people who have had the adverse event (in this case death) and determine if it was associated with receiving the vaccine. You don’t need to worry about for differences in vaccinated vs unvaccinated.
You only need to worry about confounding health variables that:
May tend to occur around the time people get vaccinated (or in the case of this study, at the time of a SARS-CoV-2 positive test) or
Occur temporally across a population, (for example most people getting vaccinated the same month then having an elevated risk of death in the winter months), but this is getting fairly technical and I have covered the SCCS methodology before for Sensible Medicine
The SCCS study design is not as well-suited for vaccine effectiveness estimates or risk-benefit analyses for multiple reasons:
Milder SARS-CoV-2 cases are less likely to be diagnosed and included in the data set
Healthy vaccinee bias: people tend to get vaccinated when healthy
Unhealthy Covid testing bias: people tend to get tested for SARS-CoV-2 when seeking medical care or not feeling well potentially totally unrelated to COVID-19.)
The study’s findings:
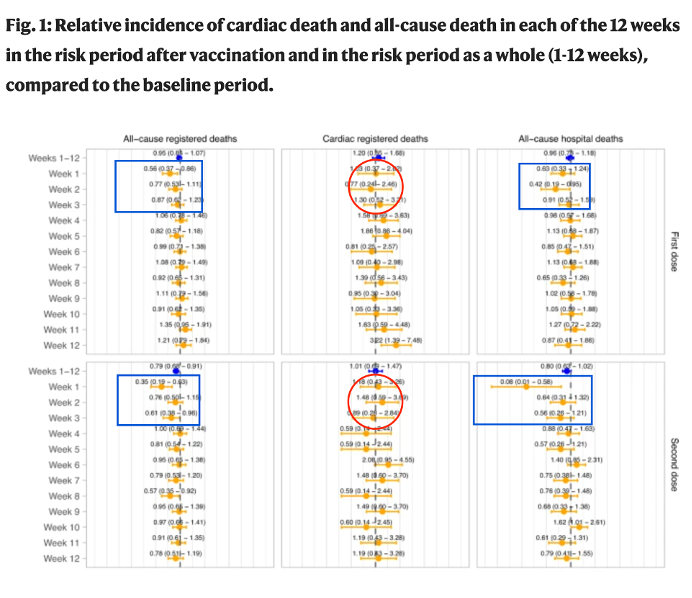
1. Healthy Vaccinee Bias
There was clear decreased incidence in all cause registered death and all cause hospital deaths immediately after vaccination. Because it is most pronounced in the first 2 weeks and only lasts 3 weeks, it’s highly implausible that it is the vaccine’s effect on COVID-19. In the first week after any vaccination, you see on the order of 40-90% decreased death incidence due to all causes (blue boxes) but interestingly, this was not seen for cardiac registered deaths (red circles) due to unclear reasons, though may in part be explained by the non-mRNA cardiac safety signal in women explained below. In any event, the healthy vaccinee bias in this study will tend to decrease the magnitude or may even entirely wash out early real harm signals from the vaccine.
2. Increased cardiac and all-cause death after dose 1 non-mRNA vaccine
The clearest finding of the paper was a 250% increased rate of cardiac death in the 12 weeks following non-mRNA vaccination in females 12-29. (which was almost exclusively Astra Zeneca with an IRR or 3.52 [1.71-7.26]). This increase in risk corresponded to 1 additional cardiac registered death for every 16,486 females in the age group vaccinated with a non-mRNA vaccine or an astounding extra 60 cardiac deaths per million. There was also an 88% increase after dose 2 non-mRNA in females as well along with smaller magnitude increases in all-cause hospital deaths. Given the timing of the administration of these vaccines, these would have either been clinically vulnerable women or healthcare workers.
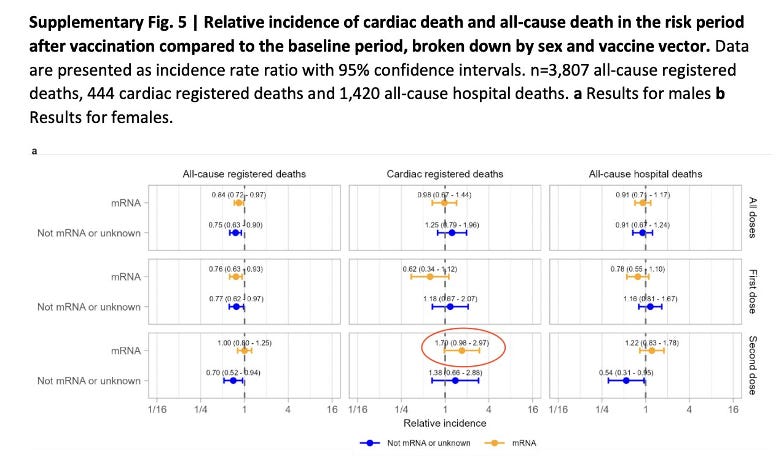
3. Increased incidence of cardiac death post dose 2 mRNA vaccine in males (which was barely non-significant)
There was also a 70% increase in cardiac death post dose 2 mRNA in males, for which the confidence interval ranged from a 2% decreased incidence to a 297% increased incidence. A 70% increase would correspond to an absolute risk of 1/360,000 second dose mRNA vaccinations in males or 2.8/million extra cardiac deaths and bear in mind the healthy vaccinee bias may have caused an underestimate of this signal.
Furthermore, remember if the real risk period lasts longer than 12 weeks, this would diminish the size of the signal at 12 weeks. The authors do state in the discussion their risk period was limited to 12 weeks due to dosing intervals and the results “suggest a negative bias with risk periods that exceeded dosing intervals”, which would indeed bias the results to underestimate vaccine-associated risks.
This supplementary figure shows incremental increases in risk period length, each estimate representing an average over a longer period of time leading up to the 12-week (total) risk period shown in orange and extending slightly beyond.
Regarding the figure above Dr. Doidge explained “Safety signals in SCCS designs should *never* be robust to specification of the risk period (because adverse event risk changes over time). It is only the *absence* of a safety signal that should be robust to this.” In other words, finding a safety signal over any time period may be grounds for concern, despite the surrounding timeframes all being non significantly elevated.
Dr. Doidge had a few thoughts on this signal in young males post dose 2 mRNA which I was able to discuss with him for the purposes of this article:
“This IRR of 1.7 (CI, 0.98-2.97) [70% increased risk] over 12 weeks… was honestly similar to the Florida study finding an 84% increase over 4 weeks.” He went on to clarify, “our effect size for male second dose was actually larger than the Florida study” [because of the longer time frame].
“Good statisticians don't get hung up on thresholds for statistical significance. Despite a competing bias, we observed a modest association in an expected combination of age group, sex, vector, dose and outcome. While there is still some uncertainty around the size of the effect, calling it spurious is either wishful thinking or willful blindness.”
“Given what we know about the prevalence of myocarditis in this subgroup, I find it very strange that people are arguing so strongly against the existence of any effect. It would have been unexpected *not* to find one. The important thing is that it's small.”
(In the conclusion, I will discuss whether or not I think it is small)
4. Increased incidence of death shortly after SARS-CoV-2 diagnosis with likely unhealthy Covid testing bias
Finally, there were large increases in all-cause and cardiac death incidences associated with SARS-CoV-2 + tests. First, because mild and asymptomatic cases are less likely to have a positive result registered, this population of SARS-CoV-2 + is not representative of the general population. Second, and more importantly, consider the circumstances under which people get tested for SARS-CoV-2. They are often getting tested because they feel sick or are receiving medical care. Thus, it is unclear exactly how much of this signal was due to SARS-CoV-2 and how much was due to other causes and the person happened to have a positive SARS-CoV-2 test. And a signal of increased risk was seen both among unvaccinated and vaccinated (but interpreting this is complex due to differences in vaccinated vs unvaccinated; this is where the “patients are their own controls” would break down in an SCCS).
Conclusions
While the rates of post-vaccination myocarditis have been easier to define, the rate of cardiac death attributable to mRNA vaccines still remains unclear. Although, with the evidence described above, in combination with the new English study, it seems unlikely the risk in this 12 week timeframe is 0 and may be closer to 3 extra cardiac deaths for every million 12-29 year olds who received a second dose of mRNA vaccine. Some may recall 3/million is also one international estimate of the overall infection fatality rate for COVID-19 in individuals under 19 years of age who had not yet been infected or vaccinated. Non-high-risk children and previously-infected children on average, would be expected to have an even lower mortality risk than that from COVID-19.
This risk to young males post dose 2 mRNA appears substantially smaller than the risk young females faced after dose 1 adenovirus vector vaccine, which was 60 extra vaccine-associated cardiac deaths per million vaccinated (though many of these women were likely to have been clinically vulnerable so this risk may not be generalizable to this age group). Both signals are more likely to be underestimates than overestimates due to healthy vaccinee bias.
I hope the results of this new study (both about non-mRNA and mRNA vaccines), the quotes from Dr. Doidge and the summary I have provided about what we have learned about post-vaccination myocarditis risks will inspire a more widespread discussion about what we actually know about COVID-19 vaccine safety and the data we should require before recommending new medical treatments including vaccines in low-risk (and really all) populations.
I have also tried to explain why direct risk-benefit analyses of COVID-19 vaccines or direct harms comparisons between vaccines and COVID-19 are inappropriate using SCCS design alone, due to substantial biases (tending to underestimate harms of the vaccine and overestimating harms of COVID-19 and vaccine effectiveness) and those diagnosed with SARS-CoV-2 being non-representative of all infected.
Due to the widespread mandates of COVID-19 vaccines among young age groups (especially when there was no good evidence of benefit to others) and ongoing COVID-19 recommendation by the CDC to low-risk groups in spite of total lack of good evidence of benefit post-infection, I think we will continue to see an interest in defining the harms vs benefits of these vaccines in different demographics – and what we knew when. I can only hope that the new movement to promote academic freedom will allow an open discussion of and lectures about the data of mRNA vaccine harms, when unnecessary harm may have occurred and the ethics of vaccination mandates in general. This would ideally result in a depoliticization of discussing and researching COVID-19 (and other) vaccine safety and efficacy- and can hopefully extend to our discussion of other controversial topics in medicine. I think this will be critical for the health of our society and individual patients alike.







An awful lot of words. Less may be better.
Here is what I want to know to start:
Pre-Covid
2015-2019 death rates from myocarditis for this particular age and gender cohort.
And all cause mortality.
Post-Covid pre-vaccination
2020 death rates from myocarditis for this particular age and gender cohort.
And all cause mortality.
Post-Covid post-vaccination availability
2021-2022 death rates from myocarditis for this particular age and gender cohort broken down by vaccination and prior infection status.
And all cause mortality.
Finding signals of low probability events can be particularly challenging. We can and will make both kinds of errors.
Finding a signal of adverse event does not tell us causation. It tells us to stop and investigate. Precautionary principle tells us we should err on side of caution. We've defaulted to 95% CIs but maybe real ethical thing to do is use 99% or even higher CIs. Clinical iatrogenesis is a real thing. Innumeracy is a problem. Hypernumeracy and randomness can also fool us.
I hope that "sensible medicine" will take up challenge of answering the question: By what method shall patients and physicians take action on the basis of probability?
Let's say risk for medical intervention is 1 micromort* risk (+\-) & for not doing intervention risk is 4 micromorts (+\-): do or not? How shall patients make decision?
*micromort = 1 in a million risk of death.
Appendicitis v appendectomy risks? How might casuistry help. Finding area of circle by inscribe and circumscribed polygons is useful exercise.
A problem especially challenging for very low probability events is the (+/-).
When is 1 in million indistinguishable from 4 in million? Any point estimate of risk has error. But breath of error and shape of error (might be non-Gaussian) is often unknown.
And in all of this, I suggest we remain cognizant of reality that patients are unique individuals. An individual who has had myocarditis before vax is not the same as person who hasn't. A person who has had some undetected adenovirus concomitant with vax is not the same as someone who hasn't. Patients who get 3/4 of vax dose or 1.5 of vax dose from distracted (whether or not well trained) healthcare provider are not the same. How about the 100 pounder vs 200 pounder. Etc.
Or for statins, is 10mg ATORVASTATIN prescribed when maybe 8 or 13mg would be better but pharma doesn't want to make pills in 1,2,4,8,16,32,64 increments (we forgot how to count in binary). How would we know?
Tracy, a major limitation of using SCCS here is if the risk of SCD in the entire period post vaccination is increased compared to pre-vaccination, then one is less likely to find an increase in risk by slicing and dicing different post-vaccination periods. So although SCCS has certain strengths, it also has significant weaknesses.