Patients with Rare Diseases Should Like the new FDA
The Study of the Week looks at Capricor Therapeutics drug for Duchenne Muscular Dystrophy. It's published in the Lancet so you can see FDA's reasoning
This morning, journalist Allysia Finley wrote a highly critical piece in the Wall Street Journal about Vinay Prasad. This was the most prominent of many criticisms directed at Dr. Prasad.
Today I will show you one of the studies the FDA rejected earlier this month. I hope to convince you that the new FDA is a positive for patients with rare diseases like Duchenne’s Muscular Dystrophy (DMD).
On July 11, FDA issued a complete response letter rejecting Capricor Therapeutics biologics license application for a drug called Deramiocel, which is a cell therapy targeting the cardiac dysfunction in DMD. FDA rejected the application because the data did not show substantial evidence of efficacy. FDA requested additional data.
Before I tell you about the study, there are two ways to think about this news. One is to think that kids with Duchenne’s just got screwed out of an available treatment. If that is your position, then it follows that we don’t need an FDA. Companies can just make something and put it on the market. And the market can decide. The other frame, the one I favor, is that we regulate new medical products for efficacy and safety.
The HOPE-2 Study
First a bit of background on Duchenne’s Muscular Dystrophy or DMD. This is a rare progressive muscle disease affecting mostly boys. The cause is a missing protein called dystrophin. Without this protective protein the muscles damage themselves with every contraction. The vast majority of children have cardiac involvement—which is severe. Life expectancy is only late teens to early 20s. It’s a really bad disease.
The proposed treatment from Capricor are cardiosphere-derived cells (name CAP-1002) which come from human donor hearts. Pieces of the donor heart are grown in culture to make progenitor cells. Unlike traditional treatments that try to fix the gene problem in DMD, CAP-1002 works through paracrine signaling--meaning the cells communicate with the patient's own cells to create healing effects. The infusions of cells are repeated every 3 months for 4 doses.
HOPE-2 authors planned to randomize more than 80 patients. They ended up enrolling just 8 patients to the active treatment and 12 to placebo. More on that later. The primary endpoint was change in mid-level elbow performance of upper limb (PUL) 1.2 score. (Recall that the drug was proposed as a therapy for cardiomyopathy.)
Authors also measured many other secondary endpoints. The primary endpoint was the only outcome prespecified for formal statistical testing.
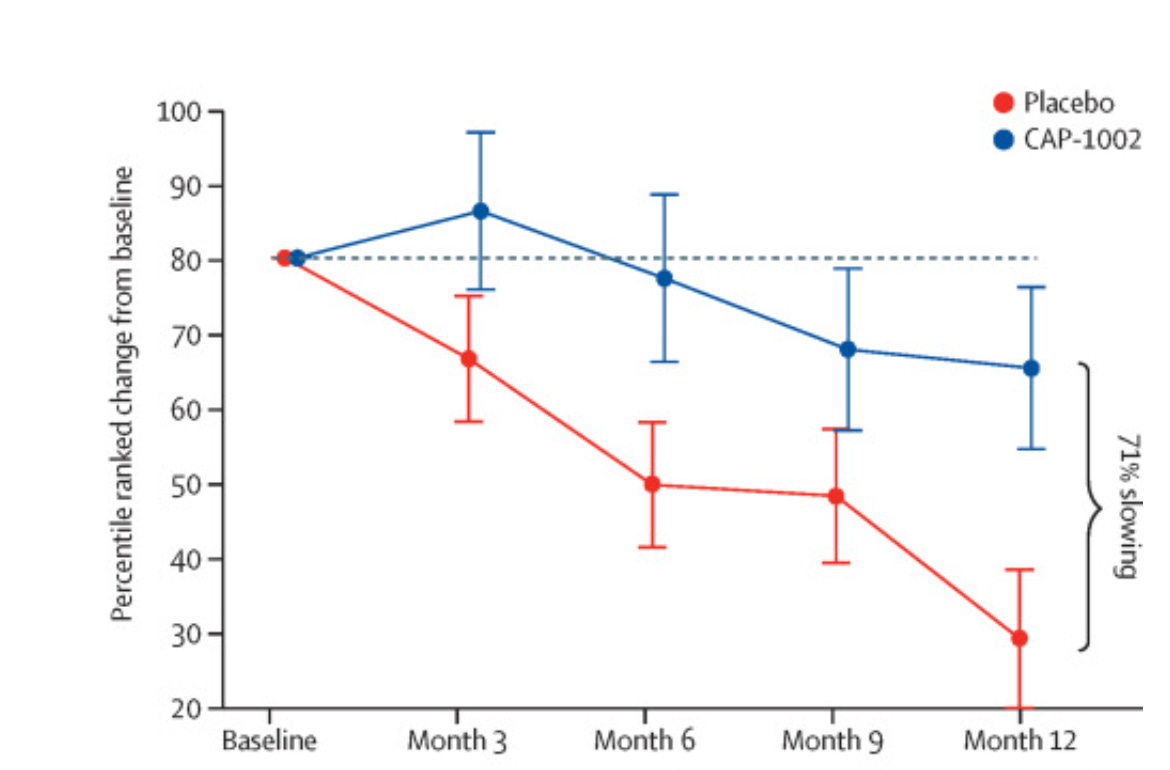
Here is a graph of the primary endpoint.
It showed a mean 12-month change from baseline in mid-level PUL 1.2, favoring CAP-1002 over placebo (percentile difference 36.2, 95% CI 7.9–64.5; difference of 2·6 points; p=0·014). “This finding represents a clinically significant 71% slowing of loss of function with CAP-1002.”
Safety: Three of the eight patients in the CAP-1002 arm had hypersensitivity reactions. One reaction required IV epinephrine and was considered serious.
Cardiac measures were made by MRI. The CAP-1002 arm had a 1% increase in LV ejection fraction. The placebo group had a mean decrease of 3.9%, leading to an effect size of ≈ 4 percentage points. Most of the MRI measures had wide confidence intervals and were not different. Notably, all strain measures did not differ. Patients in the CAP-1002 group showed a marked decrease in CK-MB as a proportion of total CK over the course of the study.
The authors concluded that the drug reduced deterioration of upper limb function. And “various measures of cardiac function and structure were improved.”
My Comments
This is somewhat encouraging data, but I completely agree it is insufficient to demonstrate efficacy. The original plan was to enroll 84 patients to have the power to show changes in upper limb function.
The trial behavior was curious. There was a plan to blindly assess results after 20 patients were enrolled—which is normal. But, then, “due to funding constraints, the trial sponsor elected to pause enrolment in the trial before the interim analysis for futility.”
Then… “based on the interim analysis and review by the data safety monitoring board, which supported lack of concerning safety signals and lack of futility, the sponsor elected to amend the protocol to reduce enrollment to the 20 already randomized patients.”
The previous FDA played a role in this decision: they recommended transitioning as quickly as possible to a phase 3 trial that would be powered based on the forthcoming 12-month HOPE-2 trial data.
I read this as saying that we need the larger phase 3 study results. So the rejection of approval this month is merely a delay until we see more data.
But I hope regular readers of Sensible Medicine can see the folly of the company trying to get the drug on the market with just HOPE-2 data.
The limitations are many:
Tiny sample size of only 8 vs 12 in the active vs placebo arms. Far below the statistical plan to enroll 84.
Short duration of only one year. If you accept the modest upper limb improvements, you would want to know it lasts longer than a year.
Nearly 40% of patients had hypersensitivity reactions. One was severe. And this occurred despite preventive measures. Safety is an obvious concern.
Patients were highly selected. Those with the most (and least) severe dysfunction were excluded
A change in LV ejection fraction of 4% points could be clinically meaningful, but with these small numbers, there is absolutely no way to tell if it is statistically robust. You would need far more patients followed for longer duration. All the cardiac measures in HOPE-2 were secondary endpoints, and the statistical tests were not adjusted for multiple looks. The same argument applies for CKMB. What’s more, LVEF is merely a surrogate measure. The ultimate measure of cardiac effects are survival and reduced hospitalizations.
My Biggest Concern – Wrong Endpoint in the Phase-3 Trial
Capricor has targeted the cardiac effects of DMD. But HOPE-2 and now the phase 3 HOPE-3 trial do not have cardiac function as a primary endpoint. Instead both will measure skeletal muscle function as the primary endpoint with cardiac measures as secondary endpoints.
If the heart is the ultimate target, why would you not design a trial to measure cardiac endpoints?
Summary
Patients with serious disease deserve proper regulatory oversight.
The bar for efficacy and safety does not have to be as high as it is for a common disease, but there needs to be a bar.
Capricor has not yet cleared any bar. The new FDA was correct to want more data than a 20-patient short-term study.



There’s a new sheriff in town and he plays by rules that prioritizes efficacy and safety. Imagine that
My blood began to boil when I read that someone was critical of Vinay Prasad even before I got to the next sentence:). I admire him greatly and was thrilled to hear about his appointment at FDA. I am biased in favor of Dr Prasad always!