The award for the most unethical control arm in prostate cancer research in 2024 goes to: ARANOTE
A Sensible Medicine Guest Post
We love it when Sensible Medicine can do better than actual journals and publish thoughtful “letters to the editor.” When one of these is also a masterful critical appraisal, all the better. This one might be a little “inside baseball,” but it is worth it for its commentary on the article and as a model for evaluating research design.
Adam Cifu
The phase 3 ARANOTE trial, which investigated the efficacy and safety of darolutamide (600 mg twice daily) plus androgen deprivation therapy (ADT) versus ADT alone in patients with metastatic hormone-sensitive prostate cancer, reaffirmed the favorable safety and tolerability profile of darolutamide observed in previous darolutamide trials (ARAMIS and ARASENS). However, the study raises several critical methodological and ethical concerns, particularly regarding the selection of the control arm, the study’s clinical relevance, and the interpretation of the findings.
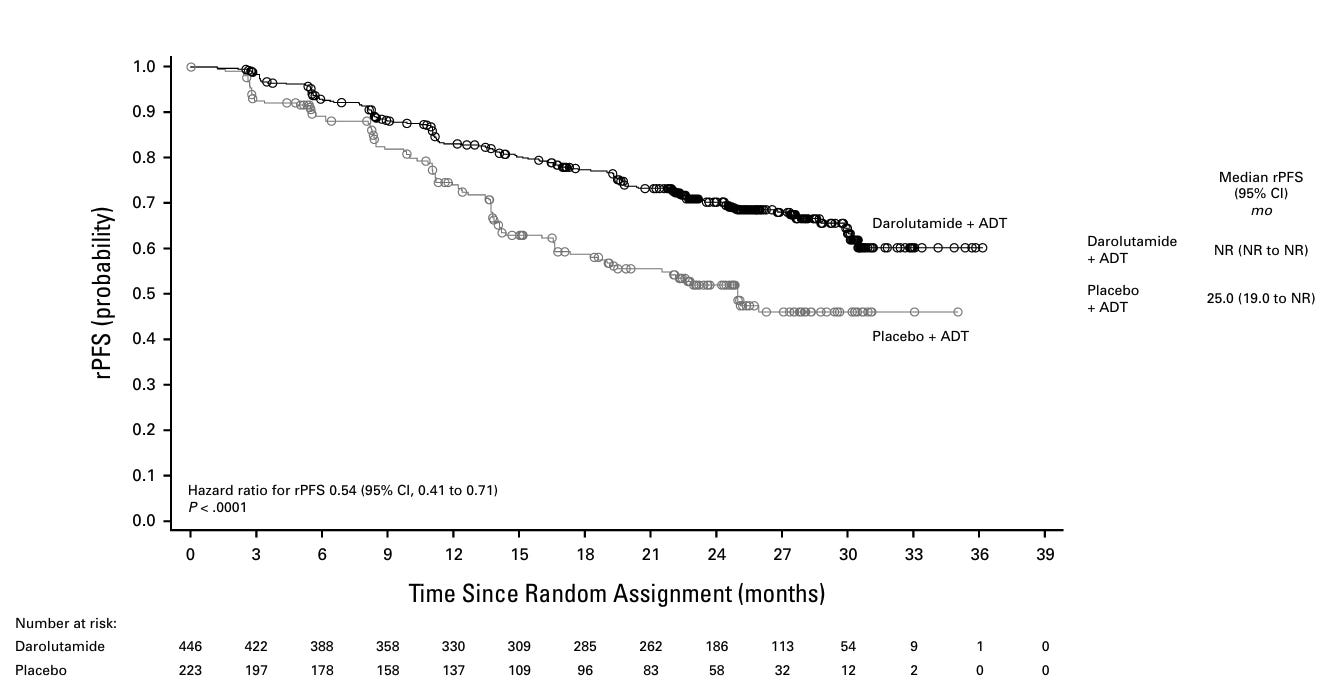
The trial demonstrated a significant improvement in radiographic progression-free survival (rPFS) with darolutamide (hazard ratio [HR], 0.54 [95% CI, 0.41 to 0.71]; P < .0001).
The overall survival (OS) results (a secondary endpoint) were also suggestive of a benefit (HR, 0.81 [95% CI, 0.59 to 1.12]). Additionally, adverse events were comparable between groups, with a lower incidence of fatigue and fewer treatment discontinuations in the darolutamide group. Based on these findings, the authors conclude that darolutamide plus ADT represents an effective and well-tolerated treatment option for patients with mHSPC.
Given the apparently positive results, why should we be concerned about this trial?
Ethical Concerns Regarding the Control Arm
The most pressing issue in the ARANOTE trial is the choice of control: ADT plus placebo. The authors acknowledge this as a limitation, yet acknowledgment alone does not justify the use of an outdated standard of care (SoC), which would constitute either ADT + androgen receptor pathway inhibitor (ARPI), ADT + taxane-based chemotherapy, or ADT + ARPI + chemotherapy. A total of 223 patients were randomized to a treatment that has been considered suboptimal since 2017–2019, following the publication of pivotal trials such as STAMPEDE (arm G), LATITUDE, ENZAMET, TITAN, and ARCHES. By the time patient enrollment began in 2021, the European Association of Urology (EAU) guidelines had already recommended against ADT monotherapy for newly diagnosed metastatic prostate cancer.
Furthermore, during the accrual phase of the ARANOTE trial, the ARASENS trial—which shares several authors with ARANOTE—established that the SoC should be triplet therapy (ADT + androgen receptor pathway inhibitor (ARPI) + docetaxel). The inconsistency between these two industry-sponsored trials is striking: while triplet therapy was promoted as the SoC in ARASENS, the control group in ARANOTE was deliberately undertreated. This raises serious ethical concerns regarding the intentional selection of an inferior control arm to demonstrate the benefit of darolutamide.
Inadequate Justification for the Control Arm
The authors attempt to justify their control arm by stating that in many enrolling countries, access to ARPIs was limited, making ADT monotherapy a commonly used treatment option. However, this argument is flawed and raises further ethical questions:
The goal of this trial was to assess the efficacy of darolutamide in metastatic hormone-sensitive prostate cancer, not to evaluate treatment strategies for resource-limited settings.
If the intent was truly to study patients without access to ARPIs, a different trial design should have been employed, focusing on improving global drug availability rather than proving efficacy against an outdated control.
If accepted as a justification for control arm selection, this reasoning could be exploited by pharmaceutical companies—designing trials in regions with limited access to modern treatments to inflate efficacy results and market expensive drugs elsewhere.
Moreover, if the intent was to introduce a more affordable alternative, the economic argument fails as well. According to the U.S. Department of Veterans Affairs, the monthly cost of darolutamide in the United States is $8,397.78, compared to apalutamide ($10,439.88), enzalutamide ($9,614.73), and abiraterone acetate ($1,607.83). Given these costs, darolutamide would still be inaccessible in resource-limited settings unless its price is significantly reduced.
Failure to Address Stated Objectives
The authors suggest that there is an unmet need for treatments that delay progression to mCRPC while maintaining a favorable safety and tolerability profile, as many patients continue to receive ADT monotherapy due to concerns about accessibility, tolerability, safety, drug-drug interactions, and physician education. However, a closer examination of the trial design reveals that ARANOTE does not adequately address these concerns.
Accessibility and Cost: A Missed Opportunity
If a large proportion of patients remain on ADT monotherapy due to financial constraints and limited access to ARPIs, then darolutamide does not solve this issue. The authors fail to acknowledge that darolutamide is one of the most expensive ARPIs available, significantly costlier than the most affordable option, abiraterone acetate.
Tolerability and Safety: No New Insights
It was already well established in ARAMIS and ARASENS that darolutamide is well tolerated, even in combination with chemotherapy. While ARANOTE confirms darolutamide’s favorable safety profile, it does not provide any new or clinically meaningful insights. The claim that darolutamide has a lower discontinuation rate than other ARPIs could have been definitively established only with an active comparator arm, rather than a placebo-controlled design.
Drug-Drug Interactions: Lack of Supporting Data
The authors claim that darolutamide has a limited potential for drug-drug interactions, making it an attractive option for elderly patients with polypharmacy. However, the trial fails to provide key data to support this claim, such as:
How many patients in the trial would have been ineligible for other ARPIs due to potential drug interactions?
What were the specific comorbidities and medications that made these patients theoretically better candidates for darolutamide?
Without real-world data on ineligibility for alternative treatments, the trial does not substantiate its claims regarding darolutamide’s superiority in this aspect.
Patient Selection and Clinical Applicability
If the true concern is that many real-world patients are not receiving ARPIs due to comorbidities, then these patients should have been included in the trial. However, the trial enrolled a highly selected population:
Median age of 70 years
97% ECOG 0-1
Required adequate bone marrow, liver, and renal function
Excluded patients with superscan metastases
These stringent inclusion criteria suggest that the study population would have been eligible for both ARPIs and chemotherapy. Thus, the trial does not reflect the real-world cohort that would benefit most from darolutamide.
Conclusion
While the ARANOTE trial provides additional data on darolutamide’s efficacy and safety, its methodological flaws limit its contribution to clinical practice. The use of an outdated control arm not only weakens the scientific validity of its findings but also raises ethical concerns regarding patient treatment and trial design. Furthermore, the trial fails to substantiate its claims regarding accessibility, tolerability, and healthcare provider education.
Dries Develtere, MD, is a Urologist at the General Hospital of Ypres, Belgium. He specializes in robotic surgery, with a focus on prostate and bladder procedures, as well as urological oncology. He is the founder of Surgical Vision, a video platform that provides high-quality surgical training videos designed to advance surgical education.



Always the seen vs the unseen. Seen: this is what we did. Unseen this is how we made things worse- ethically, theoretically and MOST importantly? For best patient outcomes in science. Such a well written piece. Thank you for taking the time to write and publish.
Benefits from the study for:
1. Investigators. Another published study for their resumes. Unknown perks from the pharmaceutical manufacturer---probably substantial.
2: Manufacturer: More hype for their product. More reprints to distribute to medical offices.
3. Patients: Nothing.