The Ideal Cholesterol Level ... Depends...And Cannot Be Determined From Observational Studies
A study making the rounds on social media reports a U-shaped association between total cholesterol and survival. It's a mess.
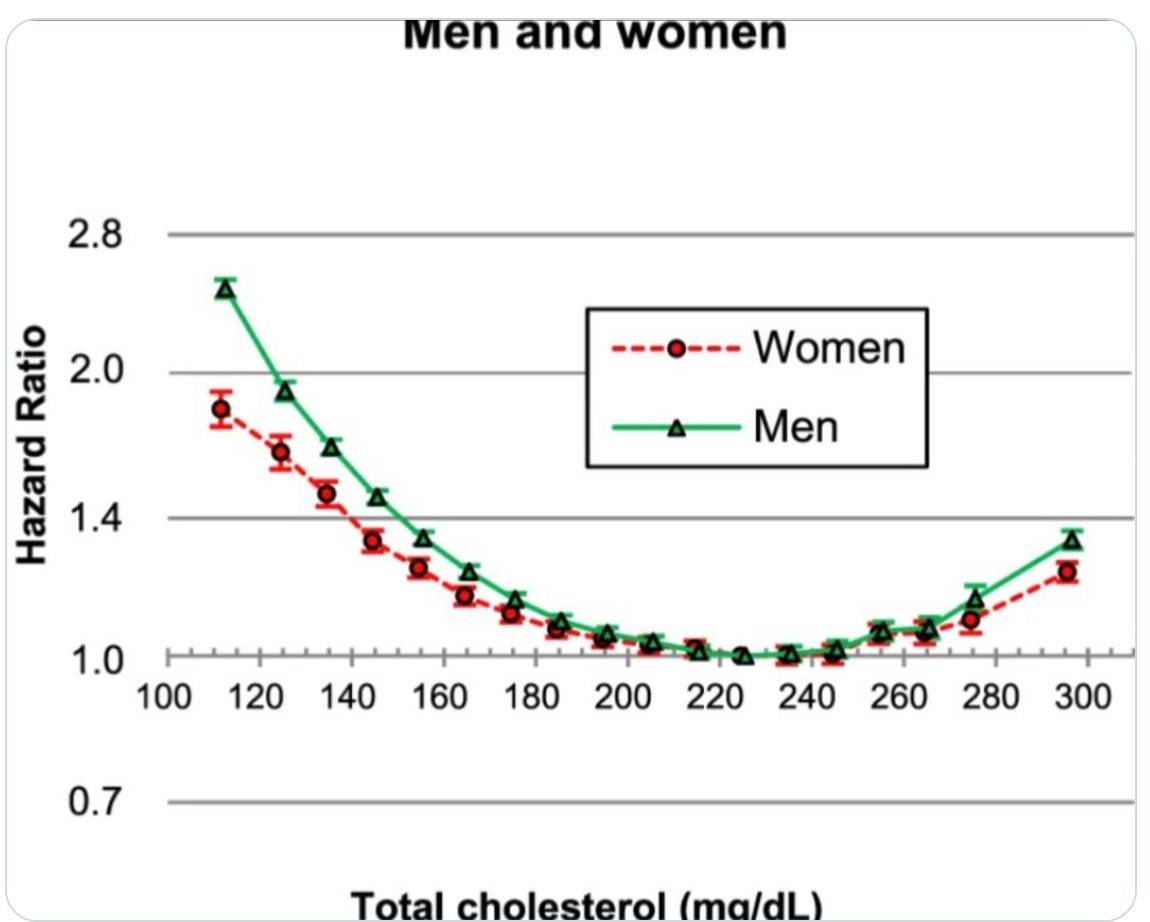
A “health coach,” who also has a quarter-million followers posted the chart below with the introduction:
This is the chart the medical and drug community doesn’t want you to understand.
Our coach goes on to write that the mainstream narrative is simple: “lower cholesterol is better. Take your statins.”
He adds:
“This chart destroys that myth. If low cholesterol really was the gold standard, why does risk of death nearly double at those levels? Cholesterol isn’t the villain. It’s an essential molecule your body uses for hormone production, vitamin D synthesis, cell membrane integrity and nervous system health.”
Coach’s errors allow for a nice teaching lesson in causal inference and evidence translation.
The Paper in Question
Nature Scientific Reports published the observational study from South Korean authors. They used big data from the national health database of nearly 13 million adults who had basic health exams from 2001-2004. They followed people for about a decade to 2013.
They made one basic correlation: total cholesterol level and death. They broke cholesterol levels into 18 categories and plotted the results.
They made minimal attempts at adjusting for variables: age, sex, smoking status, alcohol, physical activity, systolic BP, fasting glucose and BMI.
The main finding was the U-shaped relationship. Low and high cholesterol was associated with higher death rates. The slope of the lower levels was more robust than those for higher levels. A level of 220-240 mg/dl seemed ideal.
The 2019 paper was Tweeted by more than a 1000 users on X and 17 YouTube “creators” interpreted the study.
The authors concluded
TC levels <200 mg/dL may not necessarily be a sign of good health. Identification and proper management of diseases associated with lower TC levels might improve survival.
My Comments
I have little doubt that the observations are true. The problem with this paper is not the findings but the interpretation.
Inherent in the conclusion of the authors and the health coaches on the Internet is that lowering cholesterol may not be a good thing.
But this leap makes a mockery of the direction of causality.
What this observation says is that when you look at national data (all-comers) you can associate low (and high) cholesterol with a higher relative risk of death.
The famous epidemiologist Bradford Hill laid out nine criteria for determining whether an association was causal. This study violates at least 3 if not more.
First is consistency. Using the smoking and cancer analogy, the link between smoking and disease held up in different populations, time periods and types of studies
The South Korean authors state in their introduction that many other groups have published different relationships of TC and mortality.
The second Hill criteria violated by this study is coherence. The causal relationship (if present) should not contradict existing knowledge or facts about the nature of disease. Smoking, for instance, was a known carcinogen.
My explanation for why this study violates the coherence criteria: heart disease is a leading killer of people. Cholesterol is a known risk factor for heart disease and positing that low cholesterol is hazardous goes against known facts regarding the leading killer of humans.
The final and most important criteria violated by this observational study is experimental. That is, experimental evidence from randomized trials should provide strong support for the proposed causality.
If you believe the authors and health coaches that low cholesterol causes health problems, then you should be able to cite trials that show this. THERE ARE NONE.
Statins are the most studied drug ever. And these trials—with hundreds of thousands of patients—all show a consistent reduction in cardiac events and reduction of all-cause mortality.
Even the negative statin trials (CORONA in patients with heart failure and AURORA in patients on dialysis) do not suggest a harm signal.
I also know of no other total cholesterol-lowering drug that caused enough harm to support the causal claim from this observational study.
What is the likely explanation of the U-shaped curve?
The most obvious explanation is reverse causality. Instead of lower cholesterol causing higher mortality, it is likely that diseases that cause higher mortality also cause lower cholesterol levels. IOW: low cholesterol is simply a marker of illness—which leads to death.
This paper had almost no adjustment for serious illness. Cancer diagnosis was a binary yes or no. There was no information on cancer type, stage, or time since diagnosis.
This paper also had no exclusion period such that people who died shortly after baseline measurements (already ill) were not excluded. There was no information on wasting diseases, such as chronic liver, lung and kidney disease.
And there was no information on cholesterol-lowering medication. People who take these meds (and lower their cholesterol) may do so because they are ill, and had they not taken the drugs might have had even higher mortality.
Summary
The most important lesson here is to use extreme caution making causal inferences from observational studies. It’s not impossible to do so; the disease-causing properties of smoking were clearly made from observations alone.
But total cholesterol is merely a biomarker that is affected by many things.
My approach with patients who ask about cholesterol is to use pooled cohort equations that calculate 10-year risk of cardiac events. These take into account more than just a cholesterol level, things such as age, blood pressure and diabetes history.
Then we decide together whether the reduction in risk with drugs like statins aligns with their goals. We do this knowing that no study has definitively shown harm from lowering CV risk.
We don’t have trials that go for more than 5 years, so longterm risk is a bit of an unknown unknown. Professor Rodney Hayward summarizes the preference-sensitive nature of statin use quite well.
Studies such as the South Korean analysis add nothing to the uncertainty surrounding the choice to lower cholesterol levels. It should be ignored. Or used as a marker to identify people who give dodgy health advice.


What nonsense, Dr. M. Really, you should look at 100 years of health research for the simple answer on cholesterol. You are overly complicating things with your ten point questions, completely missing the main points.
There are numerous studies like this, that all show that 220 - 240 total cholesterol correlates with lowest mortality and morbidity. You can make of that what you will, but it seems clear that lowering cholesterol below 220 is a bad idea.
Cholesterol and thyroid activity go hand in hand.
The reason cholesterol is high, is due to poor thyroid function. This has been known for over 100 years. If I find a person has 280 TC, then I suggest they get their doctor to prescribe thyroid.
Their doctor prescribes nothing because he or she just has the patient get a blood test. Body temperature is the key to thyroid function as it is a proxy for metabolic rate. But doctors just pay attention to TSH, and they don’t know anything about thyroid function and have never been trained on 100 years of serious medicine.
T4 is prescribed in a few cases, and this can cause A Fib, because the body isn’t converting it into the active form of thyroid, T3. So we now have iatrogenic A Fib and cholesterol isn’t any lower anyway.
I’ve seen how easy it is for people with high cholesterol to lower it and become healthier: a good desiccated thyroid drug, or T4 and T3 BOTH.
Their metabolic rate rises, and this lowers stress hormones and makes them feel better. This is the start to better health. But not thanks to doctors who are completely ignorant of any of this established science. Shame on doctors.
The author is wrong in his statement that there are many studies showing taking statins leads to lower all cause mortality. There is at least one meta study that looked at 29 RCT done by the drug companies and in 27 of the 29 studies there was zero mortality benefit. IE the folks on Statins did not die less. So given that the author would state something so obviously wrong destroys the entire credibility of this article. Maybe the NIH should do a study that studies the effect of low cholesterol on overall mortality in a large population. As to the authors statement that the study did adjust for a whole host of other factors. If you have a population of over 13 million you have enough data not to need those factors because you’re observing the whole. If your study is on only a few hundred or even a few thousand. Then you would need to take those factors into consideration. Because one observation out of 100 can skew your results it’s called the law of big numbers. One more example of the author gas lighting in this article. One a grading scale. I am giving this one an F for attempting to gaslighting and ignoring reality.