The PISCES Trial -- A Breakthrough or Fishy Win
The nephrology and cardiology worlds are scratching their heads trying to understand how fish oil could benefit patients on dialysis that much!
NEJM published the dramatically positive PISCES trial of fish oil vs placebo (corn oil) in patients with end stage kidney disease on hemodialysis last week. I wrote a column on it for theHeart.org
I present it again today because after thinking about it all weekend, I remain confused about how this happened.
Before I tell you the details, let’s set out that trials are rarely definitive. Rather they are like medical tests, in that they update our prior beliefs. When we do a stress test on a low-risk patient with atypical chest pain, it takes a dramatically positive test for us to believe that the patient has disease.
It’s the same for fish oil in dialysis patients. We have extremely pessimistic prior beliefs for fish oil in dialysis patients. Why? Because a) it’s not clear that fish oil works in the general population. One trial was positive, the other negative. And b) nothing seems to work in dialysis patients: statins, MRA drugs, and ICDs all work in the general population but fail in dialysis patients.
Now let me show you PISCES, which was done in 26 centers in Canada.
One group gets daily supplementation with fish oil (4 g of n−3 polyunsaturated fatty acids [1.6 g of EPA and 0.8 g of DHA]) and the other group gets corn-oil placebo. (Note: corn oil placebo was used to maintain blinding, mimicking the feel of fish oil.)
The primary endpoint is serious cardiac events: sudden death, nonsudden cardiac death, MI, PVD leading to amputatin, and stroke.
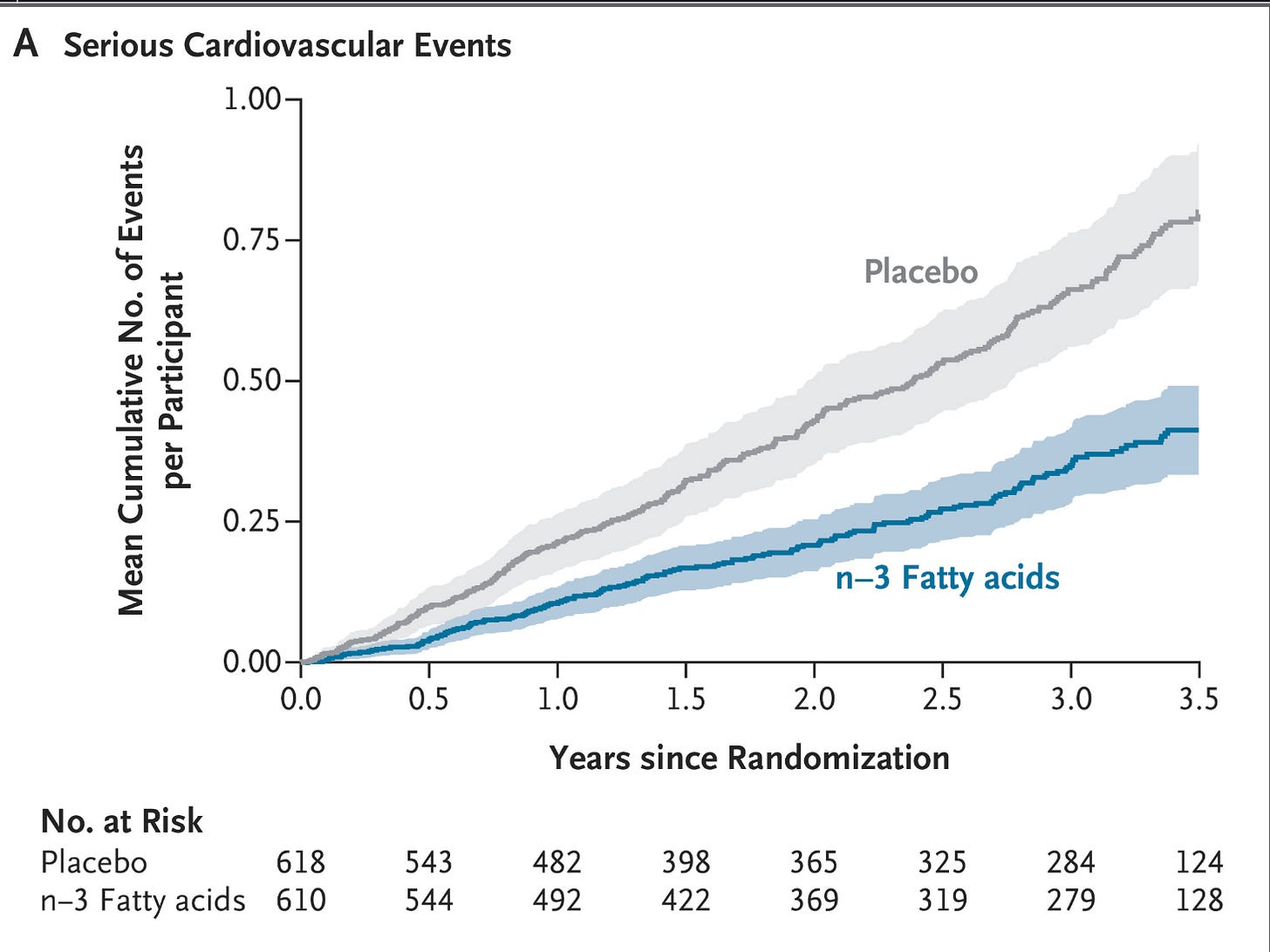
It was a home run. Here is the KM curve.
The rate of a primary outcome event was 0.31 per 1000 patient days in the fish oil group vs 0.61 per 1000 patient days (HR = 0.57; 95% CI, 0.47-0.70; P < .001).
The percentage of patients with at least one cardiovascular event appeared to be lower in the fish-oil group (20.8% [127 of 610 participants]) than in the placebo group (33.7% [208 of 618 participants]). The absolute risk reduction was 12.9%, leading to a number needed to treat to prevent one cardiac event of only 8 patients.
Here is the kicker, and something we don’t see everyday. Every component of the primary endpoint was reduced.
Cardiac death 45% lower
MI 44% lower
PVD 43% lower
Stroke 27% lower
The authors checked fatty acid levels in a sample of patients and they were significantly lower in the active arm. There were no adverse events.
Comments
Honestly, I am crowdsourcing this to Sensible Medicine readers. There’s more than a 100,000 of you. Someone must have an explanation. The trial was government funded; there seems little incentive for there to be shenanigans.
The authors spend time talking about the plausible mechanisms: dialysis patients have extremely low levels of fatty acids is one guess. Maybe.
Maybe we just missed this possibility and this is a striking new discovery. We always want confirmatory trials, but PISCES took more than a decade, so if there is one, it will be some time. Therefore, we have to decide what to do with our patients.
I did receive one interesting email from an academic cardiologist in the UK. Tell me what you think of his reasoning.
He writes:
When something seems too good to be true then it probably is, especially in a population whose cardiovascular risk is multifactorial and dominated by calcific arteriopathy and sudden death.
I think we need to look at the composite which included serious cardiovascular events which were broad and unusually included PVD leading to amputation. All these components numerically favour fish oil but there’s something methodologically suspicious: the relative risk reduction is almost uniform across all these different patho-physiologically distinct outcomes (atherothrombosis, arrhythmia, cerebrovascular, peripheral ischemia). That’s suggests either a strong unmeasured bias or an artefact of composite counting. It’s biologically implausible for omega-3s to halve risk across all these processes simultaneously.
The next problem is that death from any cause with a HR 0.89 (0.73–1.01) was not significant. Despite halving cardiac deaths the total mortality barely moved. That can’t be reconciled mechanistically unless non-CV deaths rose proportionally e.g. infection, malignancy. This undermines the plausibility of the primary finding since you can’t reduce cardiac death by half and have all-cause mortality unchanged unless classification is unstable. This implies cause-of-death attribution may have been loose, or the adjudication relied on clinical judgment without autopsy or ECG correlation.
The primary end-point events 158 vs 309 is also a problem. Multiple recurrent events are possible per patient (they mention a Williams–Peterson gap-time model), which is event-based not patient-based. If the same high-risk individuals contributed several events, an apparent “doubling” in the placebo arm can emerge from event clustering rather than genuine incidence difference. When you look at their first event analyses per person (which they show) then the numbers look more sensible: 215 vs 270; HR 0.73. So I think the main reported HR 0.57 probably overstates benefit and the first-event analysis (CV event or death 0.73 [0.61–0.87]), this is a 27% RRR which appears to me more reasonable.
This is compelling reasoning. My rebuttal might be that the components are not that disparate. If you reduce vascular outcomes you reduce PAD, MI and stroke and likely sudden death, as most sudden death is ischemic. The HR for death is not significant, but it is close. And, I do accept that adjudication of causes of death is hard. Double counting of recurring events is possible but even first events is substantially lower.
Should we be prescribing fish oil to our patients with severe chronic kidney disease on dialysis? I don’t know.
But as I wrote in my opinion column, the beauty of evidence based medicine is that how something works matters less than if something works in proper trials.
Fish oil is not super expensive, has few side effects and I would recommend it for now. But I would be little surprised if a confirmatory trial did not replicate these findings.
Let me know what you think.


I should have addressed the corn oil placebo issue. In the REDUCE IT trial of icosapent ethyl (EPA), there was a large benefit but it was against a mineral oil placebo. This was problematic because mineral oil raised LDL-C and CRP and the worry was that benefit may have simply been harm in the placebo arm.
That was the reason for corn oil. They noted that the fish oil group had elevated levels of fatty acids but corn oil did not. They also write:
"Corn oil contains approximately 50% linoleic acid (which has antiinflammatory effects) and is a source of the antioxidant vitamin E. Use of corn oil as a placebo has been associated with lower levels of serum lipids and markers of inflammation. It is possible, but unlikely, that corn oil increased the risk of cardiovascular events in the placebo group in our trial."
I would also add that in the nonsignficant STRENGTH trial, corn oil was the placebo and there were no signs of harm.
So, it's possible that corn oil could have lessened the benefit of the active arm. The problem with fish oil trials is blinding. You need something that simulates fish oil or there is no blinding.
Did anyone look at the corn oil and health? It maybe the corn oil is not good for cardiovascular health rather than fish oil being that helpful. Possibly do a similar trial with olive oil and the other 2 oils.