The VANISH 2 Trial is a Proper Study
The Study of the Week often shows you problematic studies. This week, we look at a proper study
The American Heart Association met this weekend in Chicago. A number of trials presented have serious biases. I will write about these in the coming weeks. The OPTION trial stands out as one of the most problematic. I will have a column up soon over at Medscape Cardiology. I even wrote a preview of this trial explaining its design flaws. JMM
I will try something different today. Let’s look at an exemplary study.
It’s called the VANISH 2 trial and it was presented Saturday and published in the New England Journal of Medicine.
The question is how best to handle a patient who has had a previous myocardial infarction (MI) and an implanted defibrillator and now presents with a rapid heartbeat called ventricular tachycardia. These patients often receive painful shocks from the ICD. It’s not a good situation.
VT occurs late after an MI because the occluded blood vessel causes muscle to turn to scar. But not complete scar. Within the scar, there remain channels of tissue that can conduct impulses. A premature beat can enter this scar and get stuck in the channels—like a short circuit within the scar. It results in a rapid heartbeat and potential sudden death.
There are two treatment options. One is medication. Two in particular—sotalol and amiodarone. The other treatment is to take the person to the EP lab and perform ablation within the scar that is causing the reentry of impulses.
Drugs have the advantage of being easy. You take a pill. When it works, the VT is suppressed. But drugs are not always effective and can cause adverse effects. The ablation procedure has the advantage of (potentially) being curative; but it is invasive and comes with procedural risks.
You know what comes next. The way to answer the question is randomization.
The Trial
VANISH 2 was conducted in 22 centers in Canada, the US and France. Canadian cardiologist John Sapp led the trial, which was funded mostly with Canadian government funds.
Patients were about 68 years old. The mean left ventricular ejection fraction was depressed at 34%. The trial enrolled just over 400 patients.
The next question you might be asking is about the endpoint.
The first episode of VT in patients with an ICD are rarely deadly. So you can’t measure death alone. You need other endpoints. Here they chose VT storm (where VT recurs and won’t stop), appropriate ICD shock (basically, recurrent VT) or sustained VT below the rate cutoff of the ICD.
These are good endpoints because they are not subject to bias. You are either alive or dead, or you have VT or you don’t. Unlike, say, heart failure hospitalization, no clinical decisions are required for these endpoints.
It’s important to have bias-free endpoints in an unblinded trial. In VANISH 2, patients know which group they are in.
The results
The median follow-up was quite good at 4.3 years.
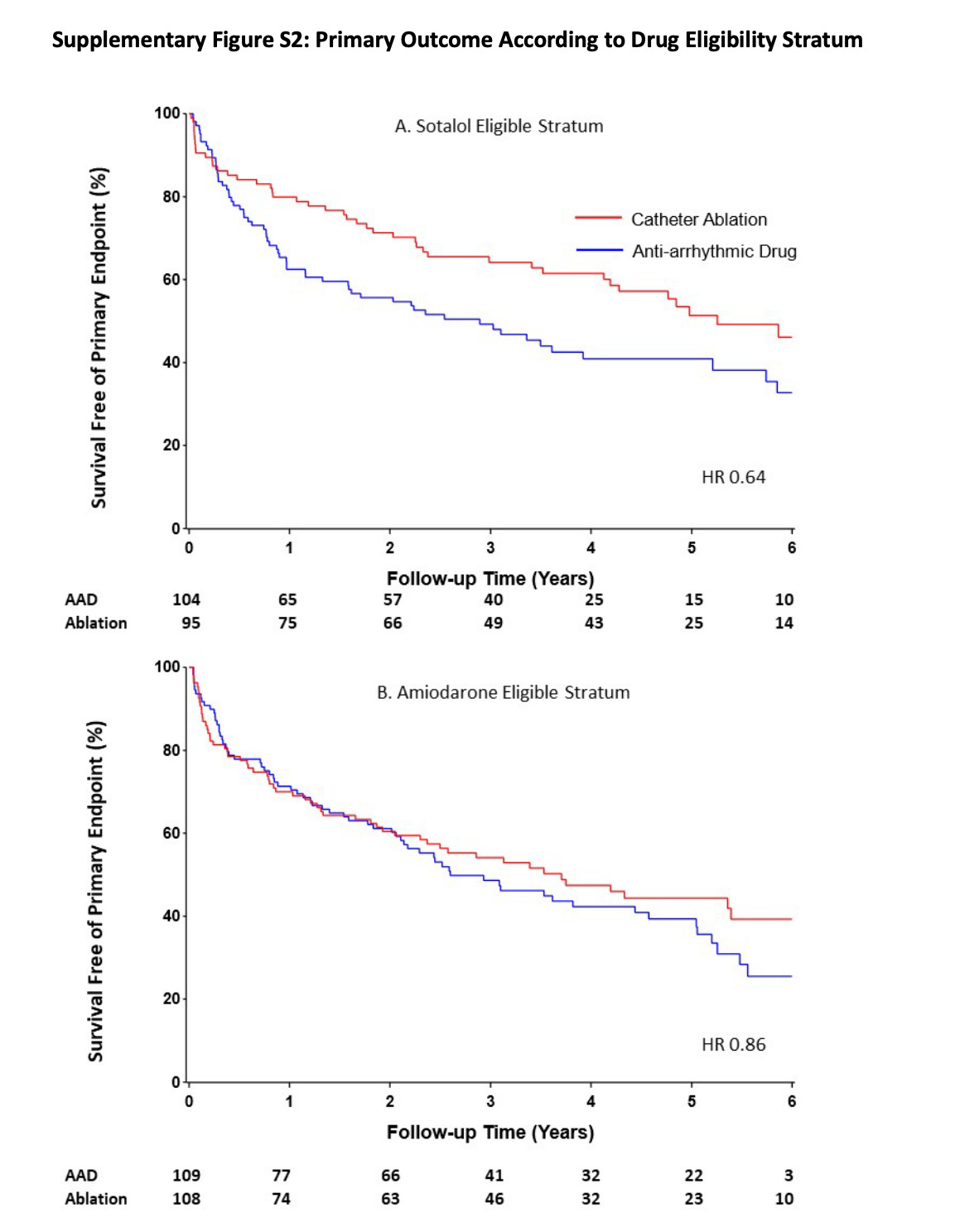
A primary end-point event occurred in 103 patients (50.7%) in the catheter ablation group and in 129 patients (60.6%) in the drug therapy group (hazard ratio, 0.75; 95% confidence interval [CI], 0.58 to 0.97; P=0.03). The graph is below.
Here are the 4 components of the primary endpoint:
Death was similar (22% vs 25%).
VT storm was similar (22% vs 23.5%)
Appropriate ICD shock was numerically lower in the ablation arm (30% vs 38%) but this did not reach statistical significance.
Treated VT below rate cutoff was much lower in the ablation arm (4% vs 16%). This outcome was the main driver of the primary endpoint.
Adverse events did occur. Adverse events within 30 days after the procedure included death in 2 patients (1.0%) and nonfatal adverse events in 23 patients (11.3%). Adverse events attributed to antiarrhythmic drug treatment included death from pulmonary toxic effects in 1 patient (0.5%) and nonfatal adverse events in 46 patients (21.6%).
I saw one important subgroup finding: Most of the beneficial effect of ablation occurred in patients who were sotalol eligible. Sotalol eligibility required numerous factors—all of which indicated a healthier patients.
Comments:
This is a well conducted study that addresses an important question. The endpoints are low in bias.
Catheter ablation reduced the risk of the composite endpoint over antiarrhythmic drugs. There were serious adverse effects in both arms. The absolute risk reduction is 10%. A number needed to treat of 10. That is a clinically relevant effect size.
Three caveats:
Most of the benefit appeared in sotalol eligible patients. These were the healthier patients who had good kidney function, little congestive heart failure and less severe VT on presentation. The reason for this heterogenous treatment effect could be because healthier patients do better with ablation, or it could be due to amiodarone being a more effective antiarrhythmic drug. I suspect future papers will explore this finding.
The main driver of the benefit came in non-fatal outcomes. Lower rates of VT under the rate cutoff of the ICD is common with antiarrhythmic drugs because the drugs also have the effect of slowing the rate of VT. Showing up with a VT at a rate of 130 BPM is not ideal, but it is almost never fatal.
The most important caveat though is that VANISH 2 was done in 22 very expert centers. VT ablation is challenging. It requires experience. Low-volume operators who spend most of their time ablating AF may not have the same skills as those in VANISH 2. We call this an external validity question. The authors did nothing wrong; external validity needs to be considered by those of us who use evidence.
VANISH 2 allows us to sit down with patients and discuss the results.
How best to apply these results turns on clinical judgement and patient values.
Before this trial there was little data to inform this decision. Congratulations to Dr Sapp and the VANISH 2 team.
P.S. I could have written this column even if catheter ablation did not prove superior to medication. The positive result is not why I congratulate the authors.




Agree with post-script. Whether a study is “positive” or not has little reflection on its quality. Good “Negative” studies can be more informative than lousy “positive” ones.
In this case, we can tell pts with ischemic CM, ICD, and VT, that ablation will reduce subsequent slow VT better than meds, but that’s about the extent of benefit. Patients can then weigh that vs upfront procedural risk, and potential risk of medication side effects. That’s a highly informative result.
When a procedural study does not have sham control, objective outcomes like VT is what we want to see….rather than subjective things like “oh some doc decided to admit you”.
Keep it simple. Excellent comment on excellent study.