Buying What SELECT is Selling: Semaglutide
A slightly skeptical read of The Skeptical Cardiologist
I am huge of fan of the The Skeptical Cardiologist, who I will refer to as TSC. His opinions are often ones I hope I would have come to if I was thinking about the same topic. His substack and twitter feed are totally worth following. I read his post last week on Sensible Medicine and agreed with pretty much everything he said. I also was left with a different conclusion. Because at Sensible Medicine we “feature contrasting ideas and opinions” and I had some time today, I thought I’d take a minute to put forward my view, maybe not quite contradictory but contrasting.
As TSG noted, SELECT showed that obese (BMI>27), non-diabetic patients with established cardiovascular disease (CVD: MI, peripheral artery disease, or stroke) did better when treated with semaglutide. Their rate of major adverse cardiovascular events was 1.5% lower than those treated with placebo (8% vs. 6.5 %).
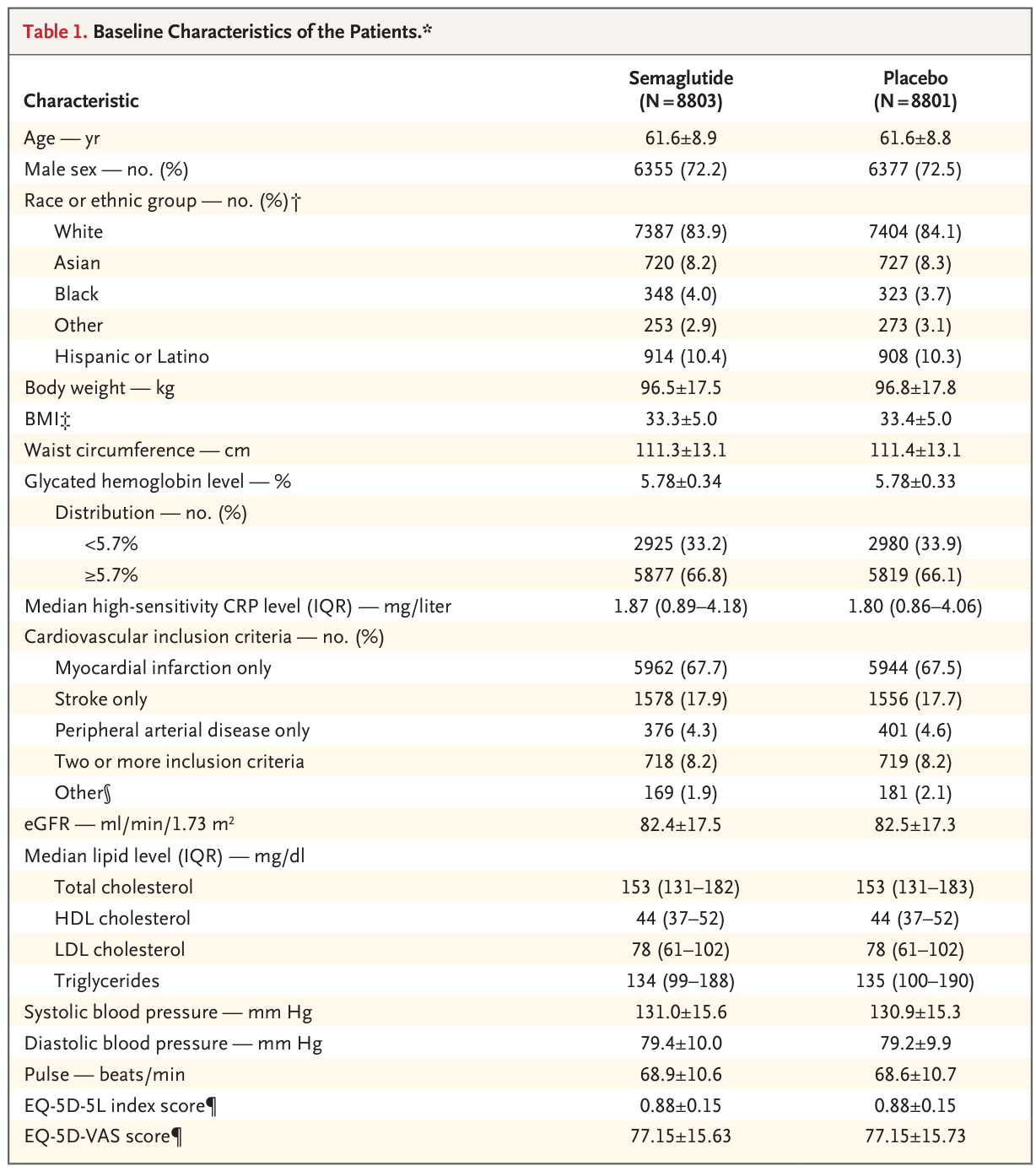
TSG’s points about the study begin with a close examination of the table 1:
He noted that these patients were not really being treated as people with established CVD should be treated. Their lipids were too high, something that could be remedied with ezetimibe. Their average hs-CRP (a measure of coronary inflammation) was elevated at 1.8, a risk factor that can be treated with colchicine. Even the blood pressure was a little too high for people with CVD.
TSC makes the totally reasonable point that you might be able to get the same CV prevention bang for your pharma buck by reaching the currently agreed upon, data-based treatment goals in these patients with widely available, relatively inexpensive drugs. I agree that might very well be true.
I think I probably agree with TSC when he says:
However, I can’t help but view the SELECT trial as cynically engineered to achieve an indication for preventing CV disease in a population that was not being appropriately treated with currently available and much more accessible therapy.
I love that quote.
I wish this study had been designed differently, in ways that no self-respecting pharma company with a new and expensive drug to hawk would design a study.
One design could have been to accept that these are real world patients who are often not treated to goal. The patients could have been randomized to reaching the treatment goals already established or to semaglutide. Besides the clinical endpoints, I would have wanted to know the costs of each strategy endpoints and (less important given the clinical endpoints) patient adherence to the meds.
Another design could have included a run-in period. Take the patients enrolled, put them through a 3-month run in period where every effort is made to reach treatment goals and then randomize them. You would sacrifice some generalizability AND some of the risk reduction.
Where I disagree is in how I think about using SELECT’s results clinically. Even if I accept that maximizing current therapy might be as beneficial as beginning semaglutide (I am not sure I do), I think my patients would/will prefer the semaglutide option. Instead of weeks/months of adding and adjusting medications, let’s add one new drug. A drug with the added benefit of weight loss in overweight patients. And, maybe after 4 years and — are you ready for this? — loss of 8% of body weight, 2.5 inches in waist circumference, and 3 points in systolic BP, maybe we can stop some of those other meds. I kind of hate to admit it, but pharma seems to be selling a pretty desirable product here.
TSC and ASC (that’s me) probably agree that the more options patients have to decrease their risk the better. With this data, a patient could choose to do nothing and accept a slightly higher risk. She could choose to work on lifestyle modification to improve her numbers and decrease her risk. She could also choose to alter her current regimen to achieve the goals we know lead to benefit. And last, she could choose to add a new, expensive drug that will lower her risk and her weight.
Let’s just hope she has a doctor who will talk her through all the possibilities.


Isn't this just another pharmaceutical con job? As a skeptical cardiologist myself, one of my firm rules is to never give figures of relative risk reduction. They are only used to sell drugs or other treatments that show such small real risk reductions that no one with any common sense would take them seriously. Granted that is logistically difficult (if not impossible) to determine risk in a disorder such as atherosclerosis that is gradually progressive with age but punctuated by acute complications (infarctions). Few drugs or studies of risk factor reduction modalities show any significant effect beyond that shown for baby aspirin (also not of any practical significance). In my opinion, we have no idea how to prevent complications of this ubiquitous process of atherosclerosis and should concentrate on improvements in treating them when they arise. There is no harm in recommending changes in "lifestyle" factors that one believes may be helpful but I draw the line at giving medications which are not only expensive but may be harmful.
I have a concern about "weight loss." I have heard discussion that a significant amount of weight loss from semaglutide is muscle loss, which I believe we would largely agree is a bad thing. Is this tracked in any of the studies being referenced? For context, I am a cancer survivor, and during chemo, I gained 22 lbs of edema on top of what had been an athletic body (active duty military). All of the information I was given about "weight gain during chemo" was actually about fat gain, and it was completely unhelpful. "Weight" can be gained or lost as fat, muscle, or fluids (at the least) and there needs to be distinctions made for healthy weight loss.