One of Cardiology’s Most Positive and Most Ignored Trials
Perhaps it was the authors' choice of a complicated name. ISAR REACT 5 doesn’t stick in your brain, like CAST, or NOAH, or PLATO. But perhaps it’s a case of marketing that has kept prasugrel down.
I present today one of the most positive trials in modern cardiology. Yet my colleagues seem to ignore it.
German authors compared two common drugs for prevention of clotting after a coronary stent in a non-industry-funded trial.
One drug won. The other lost. Yet the losing drug maintains large leads in market share. I will tell the story and hope wise commenters can help me explain the dilemma.
ISAR REACT 5 Trial
NEJM published the results of the ticagrelor vs prasugrel randomized trial in 2019.
Let’s do some brief background. The two drugs are antiplatelet agents, which are crucial after a coronary stent is placed. ISAR REACT 5 trialists enrolled only patients who were having an acute coronary syndrome—a time when coronary stents shine. Rapid opening of clot-closed coronary arteries has been modern cardiology’s greatest victory. People with heart attacks often leave the hospital the next day with a band-aid on their wrist and no major damage to their heart. (It confuses doctors and patients alike that stents used outside of acute syndromes do not provide the same benefits. But that is a story for a different day.)
The reason antiplatelet drugs are needed is that a stent is a metal cage used to prop open a blockage inside the coronary artery. Eventually the body will form a film over the metal—called endothelialization. But until then, platelets could stick to the metal and cause clot and acute vessel closure. Immediately after a stent, and for a hotly debated period of time, doctors use two antiplatelet drugs, called dual antiplatelet or DAPT. One of the drugs is always aspirin (asa).
There are three choices for DAPT: clopidogrel and asa, ticagrelor and asa or prasugrel and asa.
Clopidogrel is the Ford or Skoda of the non-aspirin antiplatelets. It’s inexpensive, once a day and often sufficient. Its Achilles heel is that genetic variations in metabolism lead to some patients having lower-than-ideal levels.
Ticagrelor is a newer antiplatelet and has been shown superior to clopidogrel in the PLATO trial, a highly controversial trial. I wrote about PLATO controversies here in December 2024. Overall bleeding rates were similar, but ticagrelor did lead to more bleeding not related to cardiac surgery, and more instances of fatal intracranial bleeding.
Prasugrel also beat clopidogrel in the large TRITON TIMI 38 trial. The relative risk reduction of 19% in major adverse cardiac events with prasugrel was muted by a 32% higher rate of major bleeding.
Bottom line: doctors reach for the more potent ticagrelor or prasugrel drugs when patients are higher risk for cardiac events after their heart attack. They try to avoid these drugs in high bleeding risk patients, but even in some high bleeding risk patients, the risk of thrombotic (clot-related) events is still greater than bleeding.
Yet ticagrelor is often the choice. Ticagrelor dominates US market share over prasugrel. And THIS IS THE MYSTERY.
The Details of ISAR REACT 5
About 4000 patients with an acute coronary syndrome (either STEMI, Non-STEMI or unstable angina) who were destined to have coronary angiography and stent placement were randomized to either prasugrel or ticagrelor.
Due to their metabolism in the body, the two drugs are given a bit differently. The loading dose of ticagrelor was given immediately after randomization; the loading dose of prasugrel was given immediately for patient having a STEMI, but it was delayed until knowing the anatomy in patients with ACS not due to STEMI.
The primary endpoint was the typical three-point MACE of death, MI or stroke at one year. Secondary endpoints including the safety endpoint of major bleeding.
Due to the excitement surrounding the PLATO trial, and, perhaps, marketing, the trialists expected ticagrelor to beat prasugrel. The power assumptions were that MACE would occur in 10% of the ticagrelor group vs 12.9% of the prasugrel group.
The trial was conducted in 21 centers in Germany and 2 in Italy. Patients were 64 years old on average with only 23% female. STEMI and NSTEMI were 41% and 46% respectively. At discharge, 81% of patients in both the ticagrelor and prasugrel groups received the randomly assigned trial drug.
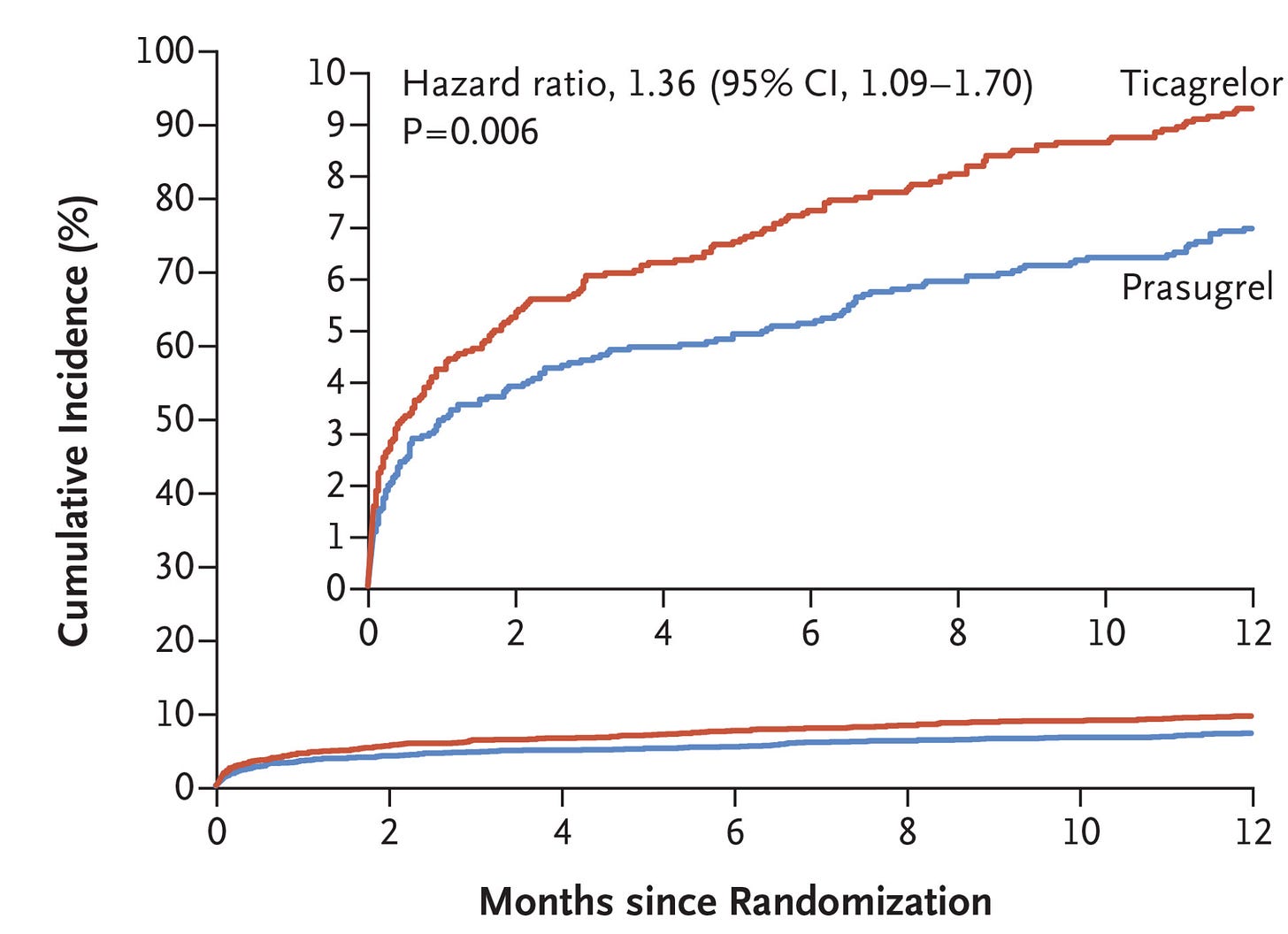
To the authors surprise, patients in the ticagrelor group had a 36% higher rate of the composite primary endpoint of death, MI and stroke. The hazard ratio of 1.39 had 95% confidence intervals from 1.09 to 1.70). The p-value of 0.006 confirmed that this clinically meaningful result was also statistically robust.
The 2.4% absolute risk reduction was also large. (9.3% vs 6.9%), leading to an NNT of 42 patients. All components of the primary endpoint favored prasugrel, though the major driver was 1.8% fewer MIs in the prasugrel arm.
Most surprising was that prasugrel achieved these reductions in hard clinical events without raising the risk of bleeding. Major bleeding occurred in 5.4% of the ticagrelor arm vs 4.8% in the prasugrel arm. HR 1.12 (0.83-1.51).
Conclusions of the authors, editorialist and a recent observational study
The authors concluded that prasugrel outperformed ticagrelor. Hani Jneid, MD, an academic interventional cardiologist at Baylor wrote in an accompanying editorial, that…(emphasis mine):
Prasugrel has now become the P2Y12 receptor inhibitor of choice in patients with acute coronary syndromes. It should be used instead of ticagrelor in appropriately selected patients with this condition.
Last year, a German-led group used insurance claims to attempt to emulate ISAR-REACT 5. They compared patients with ACS receiving either ticagrelor or prasugrel. In this non-random propensity adjusted comparison, the 24% higher rate of the death-MI-stroke endpoint with ticagrelor [hazard ratio of 1.24 (1.06-1.36)] was quite similar to ISAR REACT 5. They also found no statistically significant differences in bleeding.