Statin Benefit Does not Turn on Imaging Tests
A paper in a prominent cardiac journal that proclaims "no benefit" to statins in patients who have negative CT angiograms is flawed
The Journal JACC-Imaging has published a provocative study of statin treatment—which is one of the most studied treatments in all of modern medicine. Hungarian authors propose that statin use can be personalized based on results of a coronary CT scan.
The study is misleading, error-prone and potentially dangerous.
The Study:
Using the Hungarian health system, the authors studied (approx. 11k) patients who had coronary CT scans for symptoms between 2013-2020. The italics note that these were all patients with symptoms enough that a doctor ordered an angiogram.
The national health records allowed the team to look at statin use before and after the scan as well as keep track of major adverse cardiac events (MACE).
The main thrust of the paper was to ask the question: does the benefit (reduction of MACE) turn on the degree of CAD on the scan? Because, if the answer is yes, then that would allow for a personalized medicine approach.
The authors first report that the CTA results affected the use of statins. The presence of obstructive disease, high risk plaque, high CAC scores all associated with greater use of statins. This is not the major finding.
The next step in their analysis was to find a statin parameter. They could look at statin use vs nonuse. That’s binary. They chose a more nuanced parameter: a 10% increase in statin use. This is known because of the national data.
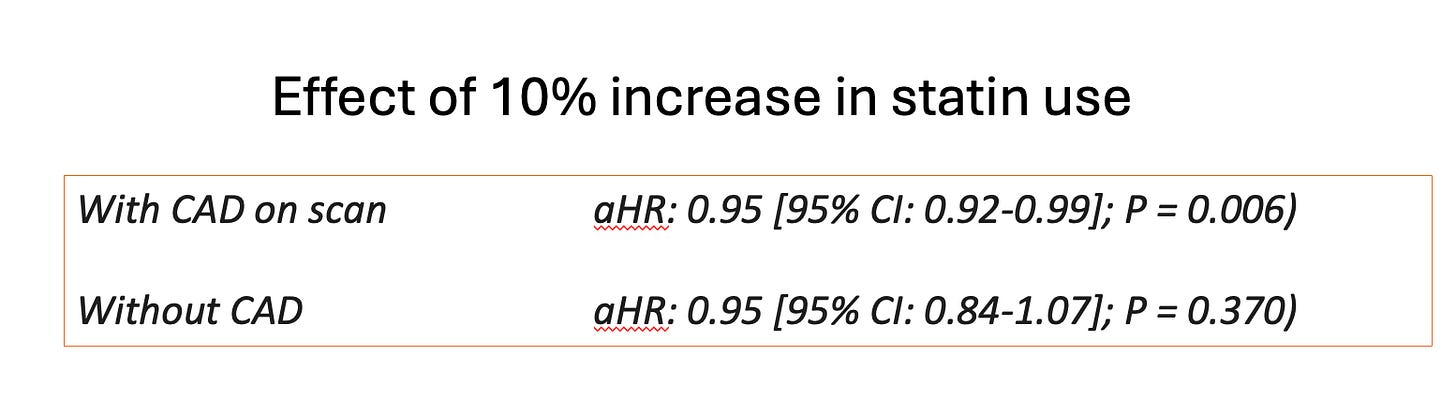
The main finding was that when they looked at a 10% increase in statin use over time after the scan, they found a statistically significant association with lower risk of MACE in patients with CAD but not in patients without CAD. I will depict this in a picture:
I hope you notice something. They write that the 10% higher statin use resulted in no reduction in MACE in patients without CAD BUT the point estimate of the HR was the same—0.95.
In both cases, the 10% increase in statins resulted in a 5% lower rate of events. The difference came in the 95% confidence intervals. There was more certainty in those with positive scans.
The next part of their paper was to look at the total population and correlate any interactions between 10% increase in statins and MACE by different findings on the CTA.
They found that a 10% increases in statins was associated with lower rates of MACE when there was
obstructive CAD (aHR: 0.91 [95% CI: 0.85-0.97]; P = 0.006),
high-risk plaque (aHR: 0.82 [95% CI: 0.68-0.98]; P = 0.026),
calcium score of ≥400 (aHR: 0.93 [95% CI: 0.87-0.99]; P = 0.024),
segment involvement score of >4 (aHR: 0.89 [95% CI: 0.84-0.95]; P < 0.001),
but not for any CAD (aHR: 0.95 [95% CI: 0.85-1.07]; P = 0.411).
The authors concluded: (I have italicized the causal language.)
Statin efficacy to decrease MACE depends on CAD phenotypes and increases with the extent and severity of disease and in the presence of high-risk plaques. Patients without CAD have no benefit from statin therapy regarding MACE. Coronary CTA may play a pivotal role in optimizing statin allocation for personalized treatment decisions to prevent MACE.
Comments:
This is a problematic analysis but even more problematic conclusion.
Before considering the specifics of the paper we should set out that hundreds of thousands of patients have been randomized in statin trials (before there were CT angiograms) and statins show a relatively consistent 20-25% reduction in non-fatal MACE.
You can quibble about the size of the absolute risk reductions; you can say that statins were not proven beneficial in dialysis and severe heart failure patients. Fine. But few evidence bases are stronger regarding the risk reduction of statins in patients without known CAD. [USPSTF meta-analysis here.]
So the conclusion that “patients without CAD have no benefit from statins” goes against more than 20 trials of statin therapy as primary prevention. When you make big conclusions, you should have strong data. This analysis is not strong data.
Problems with the Analysis:
I highlighted one above. The point estimate HR (0.95) for 10% use of statins and MACE was exactly the same whether or not there was CAD. The authors say one showed a reduction, and the other did not because one met a threshold for statistical significance. This makes a common statistical error. A more accurate conclusion would be that both point estimates of the hazard ratio the same; one had more uncertainty.
The second problem with the analysis is that a 10% statin increase is made up. What about a 5% increase, or 13% increase, or 20% increase? I ask these questions because of a clue that analytic flexibility may be substantial in this paper.
The authors tell us that in the total group, statin therapy defined as a 10% increase in statin use was protective against MACE (HR 0.95 CI 0.93-0.99). But conversely, when they defined statin therapy as any statin use (vs no statin) they write that there was no association with MACE.
But look at the HR: aHR 0.86, 95% CI 0.68-1.08) P = 0.18. This is really curious. While they write there was no association, there was actually a much larger reduction in MACE with any statin use. (14% vs 5%).
I think it’s curious because 10% more statin coverage → 5% risk reduction (HR 0.95) but going from 0% to “any” statin → 14% risk reduction (HR 0.86)
The fact that any statin (1% of the time vs 100% of the time) reduces MACE more than a 10% increase does not seem plausible. This observation suggests confounding. Namely: that those who would accept statin or increase use of statin are likely healthier, more motivated or different such that they would have lower rates of MACE.
Another clue that statin patients are different is that MACE in this case was death (3.1% of all events) and MI (0.9%). When you go into the supplement, you find similar interaction assessments between statin use and death vs MI. You’d expect statins to strongly interact with MI but not so much with death (which can occur for many non-cardiac reasons).
The fact that interaction signals between statins and death suggests that signals in this study were confounded. Healthier patients took statins.
There were other problems with the paper. Let me know in the comments.
Summary
Statin drugs reduce cardiac events by about 20-25%. If you start with a high baseline risk, such as severe CAD, you gain a greater absolute risk reduction. [.25 x 20% baseline risk is greater than .25 x 5% baseline risk]. So, I have no doubt that patients with bad CAD (on any imaging test) would sustain a risk reduction with statins.
But the authors claim of “no benefit” when no CAD is wrong. Wrong based on prior data; wrong based on their data, as both hazard ratios were 0.95, and likely wrong because their study is surely confounded by patient factors.
And the fact that “any statin” use has a much higher risk reduction than 10% increase suggests lots of analytic flexibility in this analysis.
It’s potentially dangerous to make claims like this in the scientific literature. I don’t like it. I wish peer review was stronger.
Thanks for your support. Sensible Medicine is now well over 100,000 subscribers. Adam and I are grateful. It’s shocking, really. JMM


As always, erudite and well written, thank you. But, respectfully disagree, Dr. M. First, too much causal language: “the 10% increase in statins resulted in a 5% lower rate of events.” As you know, virtually all changes in the study are likely healthy user bias, and definitely associations. Second, I beg you to reassess statin data through the lens of true benefit. The great majority of ‘benefit’ is in ‘revascularization’, something you have rightly pointed out is not a benefit at all. At primary prevention control rates mortality—the real reason patients take the drug—is totally unchanged. Meanwhile, non-fatal MI is a false and often misleading surrogate, and statin harms are very real and virtually always omitted from such discussions. Looking forward to your next piece, but fear your statin advocacy is misled by clever CTT (i.e. industry) hand-waving.
Statistical reanalysis of this study is illuminating. Sensible Medicine is doing a fine job.
The bottom line in the current conclusions about statin use for asymptomatic patients is that most accrue a mild ARR of MACE Of 3-5% over 10 years. Meaning that 95-97% of those patients receive no benefit. A fair unbiased presentation of this to patients is required to arrive at “shared decision making “.