An Important Article?
What a positive study of vagal nerve stimulation in rheumatoid arthritis might tell us about the doctor patient relationship.
There are articles that I know are unimportant. We cover many of those on the Fortnight podcast. There are articles that are so important that they immediately change my practice. Then there are articles like one published in Nature Medicine on 12/22/25, Vagus nerve-mediated neuroimmune modulation for rheumatoid arthritis: a pivotal randomized controlled trial. I think it is a modestly important article in rheumatology, but I wonder if it is a very important article in medicine, up there with the seminal articles that began to elucidate the physiology of the placebo effect.
The Study
The Nature Medicine article reported on a classic device trial with a sham control.1242 patients with rheumatoid arthritis (RA) who had an inadequate response or intolerance to maximal therapy had a vagal nerve stimulator implanted. The patients were randomized to active or sham stimulation for 3 months. All patients then received open-label stimulation for the 9 months following the 3-month comparison period. The primary endpoint was a clinical one, American College of Rheumatology 20% response (ACR20) at 3 months.
Why do this study? We know that vagus nerve activity modulates cytokine production. Its function is known to be dysregulated in RA. Specifically, tonic activity of the vagus nerve is diminished. The hypothesis was that stimulating the vagus nerve could reduce inflammation and improve RA symptoms. When the device was active, stimulation intensity was set to an upper comfort level (maximum = 2.5 mA) and a 1-minute train of pulses was delivered to the vagus nerve once daily at 10 Hz.
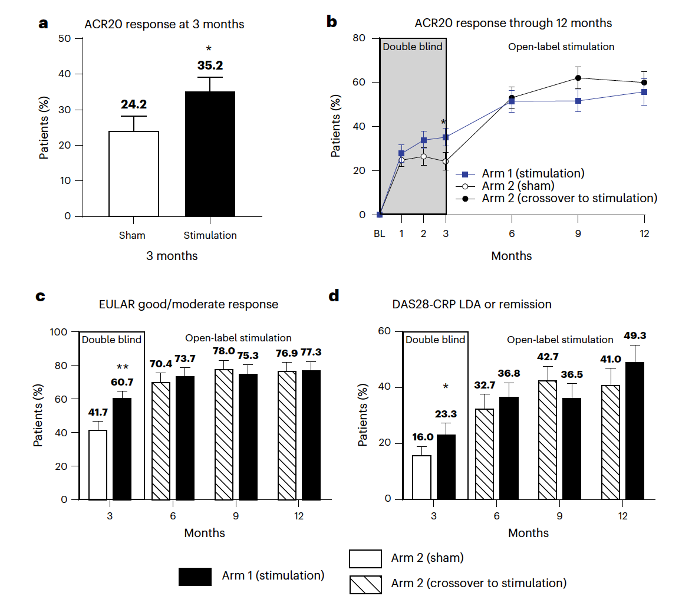
The study was positive. ACR20 rates were higher with active simulation than with sham at 3 months (35.2% versus 24.2%, P = 0.0209), and further improved to 50.0% at 6 months and 52.8% at 12 months in the open-label period. These are the primary result figures from the study:
Adverse effects were generally mild and the same in both groups. They were mostly associated with the implantation and were consistent with those seen in other devices implanted near the cervical vagus nerve – hoarseness and vocal cord paralysis being most common.
I should be satisfied with a clinical endpoint here, but I would have liked some more objective ones, such as inflammatory markers, as well. The authors did report that in “patients with high baseline risk for structural damage, active stimulation substantially reduced progression of bone erosions, as assessed by quantitative MRI joint imaging.”
My most important concern about the article is the adequacy of blinding. Blinding is most important with subjective outcomes. Although the ACR20 is well-validated, it is subjective. If the blinding was poor, or if people with an active stimulator knew they had one, the relative improvement could have been due to a placebo effect. Just polling patients with an active and inactive stimulator, asking if they thought they were in the intervention or placebo group, would have answered this concern
From a rheumatologic standpoint, this is certainly an interesting trial. It suggests that a device that stimulates the vagus nerve is effective in patients with RA not adequately controlled with current standard therapy. Vagal nerve stimulation is not without adverse effects, but it is not associated with the adverse effects seen with current biologics and targeted DMARDs. I will leave it to the rheumatologist to decide if this therapy fits into the treatment of RA. I certainly would like to see these results reproduced.
Extrapolation
What I find interesting about this study is what it suggests about how non-pharmacologic therapies might be used to treat (inflammatory) diseases. As someone who both believes in the critical importance of the doctor-patient relationship and is an evidence-based medicine fundamentalist, I have always found it frustrating that we don’t have great experimental data demonstrating that a therapeutic relationship can be, well, therapeutic.
I absolutely believe that a calm environment, such as one promoted by a good doctor-patient relationship, can benefit people’s health. I’ll give you some of the things that convince me of this:
Symptoms of Unknown Origin is a great book about inexplicable symptoms, often cured by non-pharmacologic interventions. (My favorite case is improved glycemic control achieved by adopting a cat.)
Anthony Lembo has done interesting work on delineating what aspects of a therapeutic relationship might help symptoms.
Christopher Masi generated some cool data on the relationship of autonomic tone on inflammatory markers, pregnancy outcomes, and cancer.
Here is an essay I wrote on the topic for Sensible Medicine.
I see the Nature Medicine article as a step toward showing proof of concept. If it is true that stimulating the vagus nerve with a device helps an inflammatory disease, we should push this further. Can future studies randomize people to vagus nerve stimulation, sham stimulation, and non-device stimulation? Non-device stimulation might come from a therapeutic relationship with a doctor, time with a friend, an hour of meditation, yoga, or pilates, or a morning swim in Lake Michigan.
This is a footnote worthy of David Foster Wallace. I love studies that utilize sham controls. They take the call for robust data to the ultimate extreme. I have coauthored two articles about the importance and ethics of these studies:
Why Some Patients Benefit from Participating in a Sham Surgery Trial
These are three of my favorite studies:
A Randomized Trial of Vertebroplasty for Painful Osteoporotic Vertebral Fractures
A Placebo-Controlled Trial of Percutaneous Coronary Intervention for Stable Angina
Arthroscopic Partial Meniscectomy versus Sham Surgery for a Degenerative Meniscal Tear


Dr. Cifu thank you for this post as it hits home in many ways for me. I truly enjoy this substack and of all the things I read daily in my inbox - I always look for the Sensible medicine email - always a value add and great to have civil and not nasty political debates. I don't' always agree with all the takes but I enjoy reading the "opposite view" as it expands my learning .I often share with other clinician friends that learn something and make changes in their practice and are enlightened by your analysis. Your work is important and as my Dad would say even one person can change the world. So keep it up!
In regards to this specific article, I wanted to comment on the content and how it totally hit home to me. Hopefully this won't be too rambling! Back when I was in college I had a professor who talked about how your "mind" and how you thought could improve outcomes in illness. (this was the mid 80s) At first, as a young didactic trained science major, I was skeptical. But over the years of living, practicing pharmacy (clinical practicing Pharma D in ambulatory, hospital, teaching, research and managed care), reading about therapeutics (and non western medicine especially) and as a patient myself at various times, I have come to respect this approach as a very important component in health and maybe the most important. When I went through breast cancer therapy years ago I had an amazing MD that used these techniques in addition to other medical metrics to manage my care. He became the most important person in my recovery . He was my oncologist Dr Fetting at JHU (who was also trained as a psychiatrist which I found out years later but didn't know at the time). His attentiveness, engagement, calm demeanor and caring totally changed my mental framework especially the first few years "post" treatment where most of the "support" from those around you has diminished because you are "well". but in reality it is a very fragile time. I give him a significant amount of credit for my mental and physical recovery and my lack of recurrence (20. years this year) Since then I discovered A "resort/spa" that focuses a lot on mindfulness as its main mantra for a healthy life; and I truly believe these types of approaches where we focus on these aspects of our health actually are more important than many other biological solutions. Our western society has gotten so focused on tech and science and driven away from spiritual/emotional health (mainly bc we don't truly understand or cant figure out how to measure it) that we have taken away an important part of healing. The community doctor who knows your family, knows and actually cares about you ,who can connect your history instead of looking at an error filled EMR and who actually does physical exams and listens to you is a true healer. As I always say the art of medicine is hard to put a price on and non clinicians often do not understand this. Hopefully in western medicine we will realize this and start to incorporate other "non scientist" types in medical care again and start to explore this more. To help this move forward, I believe liberal arts college degrees should be required for medical school acceptance not just science courses. We need family doctors not AI computers. Anyone who truly thinks AI will replace real medicine are misguided administrators. I pray this wont take very long to figure out - but it make take a long time for those non clinical admins to understand. Again, thanks for this post.
Thanks for sharing this interesting study, Dr. Cifu. I wrote an article about VNS a couple of years ago. Dr. Greg Plotnikoff (one of my favorite go-to sources, a truly remarkable physician) spoke with me at length about the results he was seeing in some of his patients with inflammatory conditions by using a handheld VNS device (no implantation required). One of his quotes has stuck with me: "For people who have struggled with stress and chronic inflammation for years, it offers proof to the body and mind that another state is possible." https://experiencelife.lifetime.life/article/how-to-reset-your-vagus-nerve-and-find-calm/