Tomosynthesis vs Digital Mammography Screening in Women with a Family History of Breast Cancer
One of two posts on breast cancer screening today
Today, we have “two-for”: a brief critical appraisal of a recent article on breast cancer screening modalities AND a discussion with an expert on the topic. Here is the critical appraisal. There is a second post with the podcast.
We spend a lot of time on Sensible Medicine – perhaps too much – considering the care of healthy people. We focus on this area because, as medical conservatives, we worry about turning healthy people into patients. Ideally, all medical care would be founded on robust data. This is inarguably most true when we are caring for healthy people. Overdiagnosis and overtreatment have the potential to cause real harm – physical, psychological, and financial. Some of the “care of the healthy” we’ve covered include Cancer screening, Vaccination, Cholesterol-lowering therapy, and even how caring for healthy people can harm primary care doctors.
The screening mammogram is one of the most common tests offered to healthy people. We hope that mammograms will detect breast cancer early and therefore improve outcomes (morbidity and mortality). We fear that mammograms lead to overdiagnosis and overtreatment and help only a very small number of women. To complicate matters, our trial data is outdated — everything has changed since it was collected. The population has changed, our diagnostic technology has changed, and the treatment of breast cancer has changed.
An issue that I am faced with at least weekly is the recommendation for different, or additional, screening modalities for women with dense breasts. Not surprisingly, since we don’t have modern data that delineates the risks and benefits of mammography, we also do not know the relative benefits of alternative breast cancer screening modalities.
The article, Tomosynthesis vs Digital Mammography Screening in Women with a Family History of Breast Cancer, was published in JAMA Oncology in May of 2025. This cohort study compared the performance of standard mammogram (digital mammography, DM) with that of digital breast tomosynthesis (DBT), commonly referred to as 3D mammography. In tomosynthesis, X-rays of the breast are acquired from multiple angles to create detailed, thin-slice, 3D images. Tomosynthesis uses a bit more radiation than standard mammography.
Design
This was a retrospective, observational cohort study that compared women over 18 years of age, with a family history of breast cancer (self-reported, in 1st or 2nd degree relatives) who underwent either DBT or DM screening. Outcomes were the differences between DBT and DM for recall rate, cancer detection rate, interval cancer rate, advanced cancer rate, biopsy rate, positive predictive values, sensitivity, and specificity. The data were analyzed for the entire cohort and subdivided by breast cancer family history category, breast density, age group, and screening interval (among other factors). 208, 945 women who underwent 502 357 screening examinations were included in the analysis.
Results
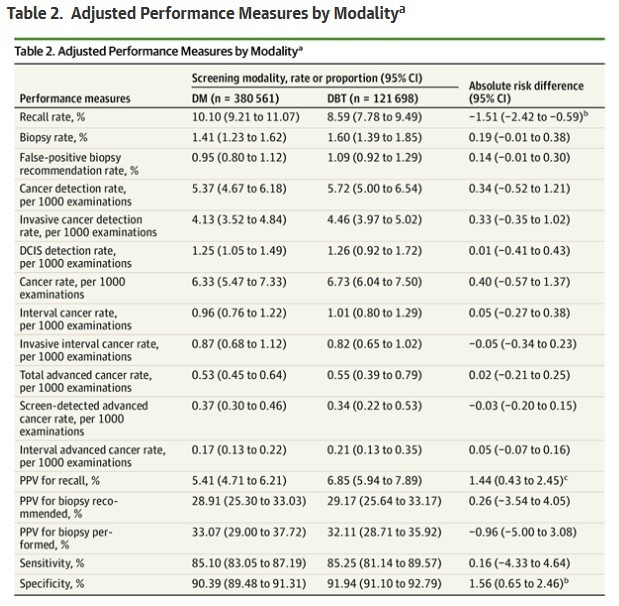
Nearly an endless number of results were reported. Some notable results follow, all are reported as adjusted absolute risk differences with 95% CIs. In the entire cohort:
The recall rate was lower for DBT vs. DM: −1.51% (−2.42% to −0.59%).
The sensitivities of the tests were the same (~85%), but the specificity was a bit higher for DBT, 91.94% vs. 90.39% (differene 1.56%; 0.65%-2.46%)
Other comparisons were not different, as seen in this table:
When comparing women with either dense or fatty (non-dense) breasts, some reported differences included:
For women with almost entirely fatty breasts, the detection rate of ductal carcinoma in situ (DCIS) was significantly lower for DBT than DM (ARD, −0.71 per 1000 examinations)
For women with scattered fibroglandular densities, the recall rate was lower (−1.90% [−2.88% to −0.92%]).
For women with scattered fibroglandular densities, the specificity was higher for DBT vs DM by 1.93%
For women with extremely dense breasts, the biopsy rate was higher with DBT by 0.48% (0.16%-0.80%), while the advanced cancer rate was lower by −0.61 per 1000 examinations.
Conclusions
A lot of work went into this study, but it is impossible to make anything of this data in terms of actual practice. This was a high-risk population, as all the women had a family history of breast cancer. Thus, extrapolation to a standard risk population is risky. More importantly, it is an observational study, so there are almost certainly confounding factors – it is not random chance whether women underwent DBT or DM. Most importantly, the endpoints considered in this study are exceedingly far removed from actual, important, clinical outcomes. Sure, it is good that one test is marginally more specific than the other one, but if more than 1000 women need to be screened to prevent one death, and in doing so, over 300 are harmed in some way, does it matter?
The answer to me is pretty clear.


I know that the prevailing view is that mammography radiation is "harmless." However, research suggests that the radiation may be harmful. I don't know if the radiation is truly harmful or not. Still, I think it is plausible that concentrating radiation into the breast tissue could cause issues, particularly in a woman who may be more genetically susceptible. Also, as a woman with cystic dense breasts, I really don't think it is a good idea to squeeze the breasts the way that they are in a mammogram. I think it is plausible that mechanical injury can occur to the breast tissue, particularly in women with cystic breasts. Finally, insurance will not cover an ultrasound or other imaging, such as thermography. Ultrasound is covered only when the woman has jumped through the mammogram hoop. Because of my dense breast tissue, I ALWAYS get called back from my mammogram and have to have an ultrasound, but I cannot just have an ultrasound. Just my thoughts about this topic. Thank you so much for all you do here on Sensible Medicine.
The issue is we all have the anecdotal experience of the one that was saved by the screening and a faceless data point is just that ?