Blue After-Visit Summaries, COVID Vaccines, and Cancer
In December 2020, South Korea changed the color of the “after visit summary” form given to every patient after they visit a physician. The white form, which had been used for years, was changed to blue, the “blue after-visit summary” (BAVS).
Over the last few years, there has been growing concern that the dye in blue paper causes cancer. There is some plausibility to this concern, as food and other dyes have been found to be carcinogenic.
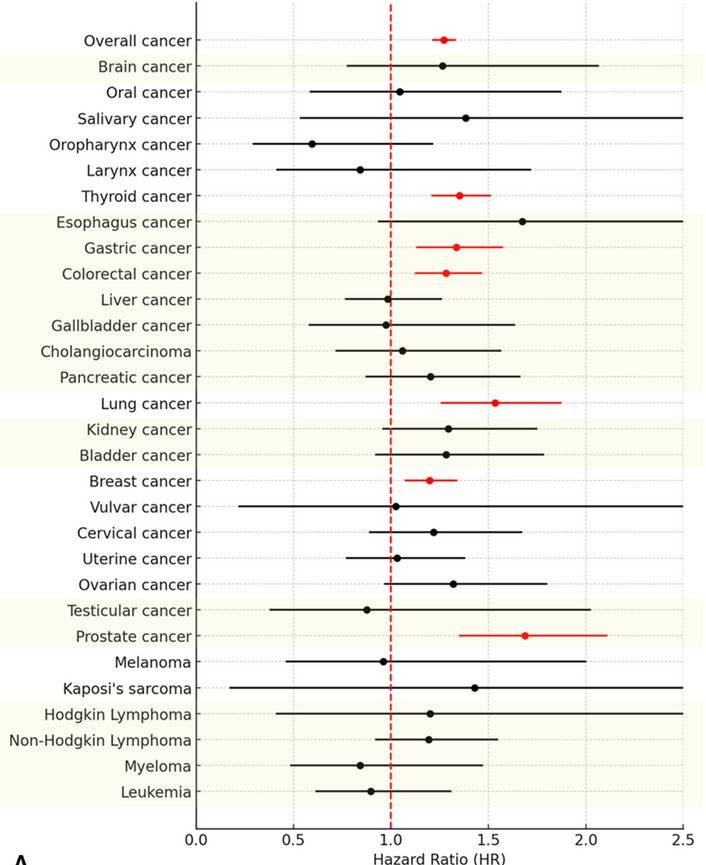
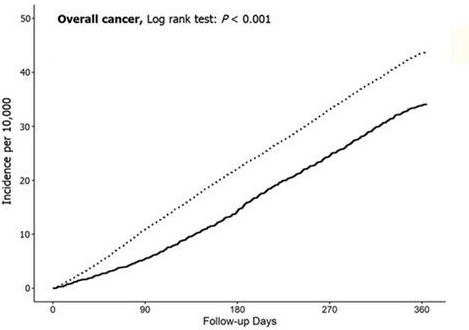
To investigate this relationship, a group of scientists compared 2,380,028 patients who had seen a doctor and received a BAVS between 2021 and 2023 with 595,007 people who had not seen a doctor and thus did not receive a BAVS. Thirty different cancer types were investigated. Six cancer types (breast, gastric, prostate, colon, thyroid, and lung) were found to be more common in the BAVS group than in the non-BAVS group. The two key figures are reproduced here.
Interestingly, the authors failed to note that the six cancers caused by BAVS are the ones commonly screened for during doctors’ visits in Korea. They do not express surprise that exposure to BAVS begins to cause cancer almost immediately after exposure (faster than is seen even after high-level radiation exposure). They also do not comment on the observation that the ill effect lasts only about 6 months—the time it might take for cancer screening tests to be scheduled, performed, and the evaluation completed. The lines on the graph above are nearly parallel after 6 months.
In fact, the authors conclude:
Considering the significantly higher risk of gastric cancer in BAVS-exposed individuals than in unexposed individuals, clinicians should prioritize monitoring the risk of gastric cancer in relation to BAVS exposure.
Of course, that is not what the authors concluded because this study did not exist. What does exist is an identical study in which the exposure of interest was a COVID booster vaccination rather than BAVS. The control group consisted of people who did not receive the vaccine (and thus may not have seen a doctor). This study, designed and analyzed exactly as the one I described above, concluded:
Considering the significantly higher risk of gastric cancer in vaccinated individuals than in unvaccinated individuals, clinicians should prioritize monitoring the risk of gastric cancer in relation to COVID-19 booster doses.
I will spend no further time discussing this study. (It was painful enough reading it a few times to write this piece.) I do not know what the authors were thinking when submitting these obviously confounded data. The fact that the effect is seen almost immediately and happens only in cancers commonly screened for in Korea is laughable. I am even more amazed that a journal (Biomarker Research, IF 11.5) published the article, let alone allowed the authors to write multiple statements suggesting causality based on confounded observational data.1 There are not even any biomarkers discussed in this article!
I have suggested that we need fewer journals; fewer journals publishing less but better research. Besides ridding the literature of meaningless, distracting, and confusing research, reducing the number of journals would have beneficial downstream effects. Physicians would spend more time caring for patients. More people would be available to peer-review worthwhile research. It would be impossible to demand that undergraduates, medical students, and residents fill their CVs with unnecessary research they would rather not doing.
Back to the COVID vaccine. Last week, I wrote about a recent article that estimated the benefits of the COVID vaccine. The study was well done, but I pointed out the flaws that meant that even the low efficacy and high number needed to vaccinate were likely overestimates of the vaccine’s effectiveness. These numbers should help people make informed decisions about whether COVID vaccination is still warranted.
That is the benefit side of the equation. The harm side of the equation is more difficult to quantify, as rare adverse effects are hard to determine and quantify. Studies like this one do us no favors.2 Because patients continue to ask for guidance on whether or not they should receive a booster vaccine, we will continue to review the data as it becomes available.
I should not be surprised. In 2013, we published an article titled: Observational studies often make clinical practice recommendations: an empirical evaluation of authors’ attitudes.
This recent release from Pfizer lists the studies of myocarditis related to vaccination.


If the blue summary study existed, I'd be curious to know whether it is assumed people keep it by their bed and read it every night for a year, or immediately drop it in the trash bin when they get home.
Great satire!
And yes, SO MANY journals need to be culled. I realize there’s an argument for “democratization” of publishing. OTOH, when you bypass the gate-keepers, you get absolute garbage like this covid study. Having said that, plenty of nonsense gets published under the big banners these days also. It’s almost as if editors simply need to wake up and start doing their jobs.